0001047335
NATIONAL HEALTHCARE CORP
false
--12-31
FY
2022
15,447,211
0.01
0.01
45,000,000
45,000,000
15,357,746
15,357,746
15,452,033
15,452,033
3,728,000
20
40
3
15
2
15
0
477
10
0
0
0
10
2
5
0
0
1,084,763
1,084,763
1
120
10
5
5
11,047,000
11,047,000
00010473352022-01-012022-12-31
iso4217:USD
00010473352022-06-30
xbrli:shares
00010473352023-02-06
thunderdome:item
00010473352021-01-012021-12-31
00010473352020-01-012020-12-31
iso4217:USDxbrli:shares
00010473352022-12-31
00010473352021-12-31
00010473352020-12-31
00010473352019-12-31
0001047335us-gaap:CommonStockMember2019-12-31
0001047335us-gaap:AdditionalPaidInCapitalMember2019-12-31
0001047335us-gaap:RetainedEarningsMember2019-12-31
0001047335us-gaap:AccumulatedOtherComprehensiveIncomeMember2019-12-31
0001047335us-gaap:NoncontrollingInterestMember2019-12-31
0001047335us-gaap:CommonStockMember2020-01-012020-12-31
0001047335us-gaap:AdditionalPaidInCapitalMember2020-01-012020-12-31
0001047335us-gaap:RetainedEarningsMember2020-01-012020-12-31
0001047335us-gaap:AccumulatedOtherComprehensiveIncomeMember2020-01-012020-12-31
0001047335us-gaap:NoncontrollingInterestMember2020-01-012020-12-31
0001047335us-gaap:CommonStockMember2020-12-31
0001047335us-gaap:AdditionalPaidInCapitalMember2020-12-31
0001047335us-gaap:RetainedEarningsMember2020-12-31
0001047335us-gaap:AccumulatedOtherComprehensiveIncomeMember2020-12-31
0001047335us-gaap:NoncontrollingInterestMember2020-12-31
0001047335us-gaap:CommonStockMember2021-01-012021-12-31
0001047335us-gaap:AdditionalPaidInCapitalMember2021-01-012021-12-31
0001047335us-gaap:RetainedEarningsMember2021-01-012021-12-31
0001047335us-gaap:AccumulatedOtherComprehensiveIncomeMember2021-01-012021-12-31
0001047335us-gaap:NoncontrollingInterestMember2021-01-012021-12-31
0001047335us-gaap:CommonStockMember2021-12-31
0001047335us-gaap:AdditionalPaidInCapitalMember2021-12-31
0001047335us-gaap:RetainedEarningsMember2021-12-31
0001047335us-gaap:AccumulatedOtherComprehensiveIncomeMember2021-12-31
0001047335us-gaap:NoncontrollingInterestMember2021-12-31
0001047335us-gaap:CommonStockMember2022-01-012022-12-31
0001047335us-gaap:AdditionalPaidInCapitalMember2022-01-012022-12-31
0001047335us-gaap:RetainedEarningsMember2022-01-012022-12-31
0001047335us-gaap:AccumulatedOtherComprehensiveIncomeMember2022-01-012022-12-31
0001047335us-gaap:NoncontrollingInterestMember2022-01-012022-12-31
0001047335us-gaap:CommonStockMember2022-12-31
0001047335us-gaap:AdditionalPaidInCapitalMember2022-12-31
0001047335us-gaap:RetainedEarningsMember2022-12-31
0001047335us-gaap:AccumulatedOtherComprehensiveIncomeMember2022-12-31
0001047335us-gaap:NoncontrollingInterestMember2022-12-31
xbrli:pure
0001047335nhc:ImpairmentRecoveryOfAssetsMember2022-01-012022-12-31
0001047335nhc:ImpairmentRecoveryOfAssetsMember2021-01-012021-12-31
utr:Y
0001047335us-gaap:BuildingAndBuildingImprovementsMembersrt:MinimumMember2022-01-012022-12-31
0001047335us-gaap:BuildingAndBuildingImprovementsMembersrt:MaximumMember2022-01-012022-12-31
0001047335nhc:EquipmentAndFurnitureMembersrt:MinimumMember2022-01-012022-12-31
0001047335nhc:EquipmentAndFurnitureMembersrt:MaximumMember2022-01-012022-12-31
0001047335srt:MinimumMember2022-12-31
0001047335srt:MaximumMember2022-12-31
0001047335nhc:RefundableAdvanceFeesMember2022-01-012022-12-31
0001047335nhc:OriginalEntryFeeMember2022-01-012022-12-31
0001047335nhc:AppreciationMember2022-01-012022-12-31
0001047335nhc:ProviderReliefFundUnderCARESActMember2022-01-012022-12-31
0001047335nhc:ProviderReliefFundUnderCARESActMember2021-01-012021-12-31
0001047335nhc:ProviderReliefFundUnderCARESActMember2020-01-012020-12-31
00010473352020-04-012020-06-30
0001047335nhc:SupplementalMedicaidPaymentsMember2022-01-012022-12-31
0001047335nhc:SupplementalMedicaidPaymentsMember2021-01-012021-12-31
0001047335nhc:SupplementalMedicaidPaymentsMember2020-01-012020-12-31
0001047335nhc:InpatientServicesMember2022-01-012022-12-31
0001047335nhc:InpatientServicesMember2021-01-012021-12-31
0001047335nhc:InpatientServicesMember2020-01-012020-12-31
0001047335nhc:HomecareAndHospiceServicesMember2022-01-012022-12-31
0001047335nhc:HomecareAndHospiceServicesMember2021-01-012021-12-31
0001047335nhc:HomecareAndHospiceServicesMember2020-01-012020-12-31
0001047335nhc:MedicareMember2022-01-012022-12-31
0001047335nhc:MedicareMember2021-01-012021-12-31
0001047335nhc:MedicareMember2020-01-012020-12-31
0001047335nhc:ManagedCareMember2022-01-012022-12-31
0001047335nhc:ManagedCareMember2021-01-012021-12-31
0001047335nhc:ManagedCareMember2020-01-012020-12-31
0001047335nhc:MedicaidMember2022-01-012022-12-31
0001047335nhc:MedicaidMember2021-01-012021-12-31
0001047335nhc:MedicaidMember2020-01-012020-12-31
0001047335nhc:PrivatePayAndOtherMember2022-01-012022-12-31
0001047335nhc:PrivatePayAndOtherMember2021-01-012021-12-31
0001047335nhc:PrivatePayAndOtherMember2020-01-012020-12-31
0001047335nhc:MedicareAndMedicaidMember2022-12-31
0001047335nhc:MedicareAndMedicaidMember2021-12-31
0001047335stpr:FL2022-12-31
0001047335nhc:NationalMember2022-12-31
0001047335nhc:NationalMember2022-01-012022-12-31
0001047335nhc:NationalMember2021-01-012021-12-31
0001047335nhc:NationalMember2020-01-012020-12-31
0001047335nhc:NationalMember2021-12-31
0001047335nhc:ManagementServicesProvidedToOtherFacilitiesMember2022-01-012022-12-31
0001047335nhc:ManagementServicesProvidedToOtherFacilitiesMember2021-01-012021-12-31
0001047335nhc:ManagementServicesProvidedToOtherFacilitiesMember2020-01-012020-12-31
0001047335nhc:WorkersCompensationRevenueMember2022-01-012022-12-31
0001047335nhc:WorkersCompensationRevenueMember2021-01-012021-12-31
0001047335nhc:WorkersCompensationRevenueMember2020-01-012020-12-31
0001047335us-gaap:ProfessionalLiabilityInsuranceMember2022-01-012022-12-31
0001047335us-gaap:ProfessionalLiabilityInsuranceMember2021-01-012021-12-31
0001047335us-gaap:ProfessionalLiabilityInsuranceMember2020-01-012020-12-31
0001047335nhc:AcquisitionOfCarisMember2021-06-11
0001047335nhc:AcquisitionOfCarisMember2020-12-31
0001047335nhc:InpatientServicesSegmentMember2022-01-012022-12-31
0001047335nhc:HomecareServicesSegmentMember2022-01-012022-12-31
0001047335us-gaap:AllOtherSegmentsMember2022-01-012022-12-31
0001047335nhc:InpatientServicesSegmentMember2021-01-012021-12-31
0001047335nhc:HomecareServicesSegmentMember2021-01-012021-12-31
0001047335us-gaap:AllOtherSegmentsMember2021-01-012021-12-31
0001047335nhc:InpatientServicesSegmentMember2020-01-012020-12-31
0001047335nhc:HomecareServicesSegmentMember2020-01-012020-12-31
0001047335us-gaap:AllOtherSegmentsMember2020-01-012020-12-31
0001047335nhc:TwoLeasesWithNHIMember2022-12-31
0001047335nhc:LeaseOneWithNhiMember2022-12-31
0001047335nhc:NHILeaseAgreementMember2022-09-01
0001047335nhc:NHILeaseAgreementMember2022-09-012022-09-01
0001047335nhc:NHILeaseAgreementMember2022-08-31
0001047335nhc:BothNHILeaseAgreementsMember2022-01-012022-12-31
0001047335nhc:BothNHILeaseAgreementsMember2021-01-012021-12-31
0001047335nhc:BothNHILeaseAgreementsMember2020-01-012020-12-31
0001047335nhc:SeniorHealthcareFacilitiesMember2022-12-31
0001047335nhc:SeniorHealthcareFacilitiesMember2022-01-012022-12-31
0001047335nhc:BuildingsAndPersonalPropertyMember2022-12-31
0001047335nhc:BuildingsAndPersonalPropertyMember2021-12-31
0001047335nhc:NetPropertyAndEquipmentMember2022-12-31
0001047335nhc:NetPropertyAndEquipmentMember2021-12-31
0001047335us-gaap:EmployeeStockOptionMember2022-01-012022-12-31
0001047335us-gaap:EmployeeStockOptionMember2021-01-012021-12-31
0001047335us-gaap:EmployeeStockOptionMember2020-01-012020-12-31
0001047335us-gaap:EquitySecuritiesMember2022-12-31
0001047335us-gaap:EquitySecuritiesMember2021-12-31
0001047335us-gaap:CorporateDebtSecuritiesMember2022-12-31
0001047335us-gaap:CorporateDebtSecuritiesMember2021-12-31
0001047335us-gaap:AssetBackedSecuritiesMember2022-12-31
0001047335us-gaap:AssetBackedSecuritiesMember2021-12-31
0001047335us-gaap:USGovernmentCorporationsAndAgenciesSecuritiesMember2022-12-31
0001047335us-gaap:USGovernmentCorporationsAndAgenciesSecuritiesMember2021-12-31
0001047335us-gaap:USStatesAndPoliticalSubdivisionsMember2022-12-31
0001047335us-gaap:USStatesAndPoliticalSubdivisionsMember2021-12-31
0001047335nhc:NHICommonStockMember2022-12-31
0001047335nhc:NHICommonStockMember2021-12-31
0001047335us-gaap:FairValueMeasurementsRecurringMember2022-12-31
0001047335us-gaap:FairValueInputsLevel1Memberus-gaap:FairValueMeasurementsRecurringMember2022-12-31
0001047335us-gaap:FairValueInputsLevel2Memberus-gaap:FairValueMeasurementsRecurringMember2022-12-31
0001047335us-gaap:FairValueMeasurementsRecurringMemberus-gaap:EquitySecuritiesMember2022-12-31
0001047335us-gaap:FairValueInputsLevel1Memberus-gaap:FairValueMeasurementsRecurringMemberus-gaap:EquitySecuritiesMember2022-12-31
0001047335us-gaap:FairValueInputsLevel2Memberus-gaap:FairValueMeasurementsRecurringMemberus-gaap:EquitySecuritiesMember2022-12-31
0001047335us-gaap:FairValueMeasurementsRecurringMemberus-gaap:CorporateDebtSecuritiesMember2022-12-31
0001047335us-gaap:FairValueInputsLevel1Memberus-gaap:FairValueMeasurementsRecurringMemberus-gaap:CorporateDebtSecuritiesMember2022-12-31
0001047335us-gaap:FairValueInputsLevel2Memberus-gaap:FairValueMeasurementsRecurringMemberus-gaap:CorporateDebtSecuritiesMember2022-12-31
0001047335us-gaap:FairValueMeasurementsRecurringMemberus-gaap:AssetBackedSecuritiesMember2022-12-31
0001047335us-gaap:FairValueInputsLevel1Memberus-gaap:FairValueMeasurementsRecurringMemberus-gaap:AssetBackedSecuritiesMember2022-12-31
0001047335us-gaap:FairValueInputsLevel2Memberus-gaap:FairValueMeasurementsRecurringMemberus-gaap:AssetBackedSecuritiesMember2022-12-31
0001047335us-gaap:FairValueMeasurementsRecurringMemberus-gaap:USTreasurySecuritiesMember2022-12-31
0001047335us-gaap:FairValueInputsLevel1Memberus-gaap:FairValueMeasurementsRecurringMemberus-gaap:USTreasurySecuritiesMember2022-12-31
0001047335us-gaap:FairValueInputsLevel2Memberus-gaap:FairValueMeasurementsRecurringMemberus-gaap:USTreasurySecuritiesMember2022-12-31
0001047335us-gaap:FairValueMeasurementsRecurringMemberus-gaap:USStatesAndPoliticalSubdivisionsMember2022-12-31
0001047335us-gaap:FairValueInputsLevel1Memberus-gaap:FairValueMeasurementsRecurringMemberus-gaap:USStatesAndPoliticalSubdivisionsMember2022-12-31
0001047335us-gaap:FairValueInputsLevel2Memberus-gaap:FairValueMeasurementsRecurringMemberus-gaap:USStatesAndPoliticalSubdivisionsMember2022-12-31
0001047335us-gaap:FairValueMeasurementsRecurringMember2021-12-31
0001047335us-gaap:FairValueInputsLevel1Memberus-gaap:FairValueMeasurementsRecurringMember2021-12-31
0001047335us-gaap:FairValueInputsLevel2Memberus-gaap:FairValueMeasurementsRecurringMember2021-12-31
0001047335us-gaap:FairValueMeasurementsRecurringMemberus-gaap:EquitySecuritiesMember2021-12-31
0001047335us-gaap:FairValueInputsLevel1Memberus-gaap:FairValueMeasurementsRecurringMemberus-gaap:EquitySecuritiesMember2021-12-31
0001047335us-gaap:FairValueInputsLevel2Memberus-gaap:FairValueMeasurementsRecurringMemberus-gaap:EquitySecuritiesMember2021-12-31
0001047335us-gaap:FairValueMeasurementsRecurringMemberus-gaap:CorporateDebtSecuritiesMember2021-12-31
0001047335us-gaap:FairValueInputsLevel1Memberus-gaap:FairValueMeasurementsRecurringMemberus-gaap:CorporateDebtSecuritiesMember2021-12-31
0001047335us-gaap:FairValueInputsLevel2Memberus-gaap:FairValueMeasurementsRecurringMemberus-gaap:CorporateDebtSecuritiesMember2021-12-31
0001047335us-gaap:FairValueMeasurementsRecurringMemberus-gaap:AssetBackedSecuritiesMember2021-12-31
0001047335us-gaap:FairValueInputsLevel1Memberus-gaap:FairValueMeasurementsRecurringMemberus-gaap:AssetBackedSecuritiesMember2021-12-31
0001047335us-gaap:FairValueInputsLevel2Memberus-gaap:FairValueMeasurementsRecurringMemberus-gaap:AssetBackedSecuritiesMember2021-12-31
0001047335us-gaap:FairValueMeasurementsRecurringMemberus-gaap:USTreasurySecuritiesMember2021-12-31
0001047335us-gaap:FairValueInputsLevel1Memberus-gaap:FairValueMeasurementsRecurringMemberus-gaap:USTreasurySecuritiesMember2021-12-31
0001047335us-gaap:FairValueInputsLevel2Memberus-gaap:FairValueMeasurementsRecurringMemberus-gaap:USTreasurySecuritiesMember2021-12-31
0001047335us-gaap:FairValueMeasurementsRecurringMemberus-gaap:USStatesAndPoliticalSubdivisionsMember2021-12-31
0001047335us-gaap:FairValueInputsLevel1Memberus-gaap:FairValueMeasurementsRecurringMemberus-gaap:USStatesAndPoliticalSubdivisionsMember2021-12-31
0001047335us-gaap:FairValueInputsLevel2Memberus-gaap:FairValueMeasurementsRecurringMemberus-gaap:USStatesAndPoliticalSubdivisionsMember2021-12-31
0001047335nhc:InpatientServicesSegmentMember2019-12-31
0001047335nhc:HomecareAndHospiceSegmentMember2019-12-31
0001047335nhc:HomecareAndHospiceSegmentMember2020-01-012020-12-31
0001047335nhc:InpatientServicesSegmentMember2020-12-31
0001047335nhc:HomecareAndHospiceSegmentMember2020-12-31
0001047335nhc:HomecareAndHospiceSegmentMember2021-01-012021-12-31
0001047335nhc:InpatientServicesSegmentMember2021-12-31
0001047335nhc:HomecareAndHospiceSegmentMember2021-12-31
0001047335nhc:HomecareAndHospiceSegmentMember2022-01-012022-12-31
0001047335nhc:InpatientServicesSegmentMember2022-12-31
0001047335nhc:HomecareAndHospiceSegmentMember2022-12-31
0001047335nhc:AcquisitionOfCarisMemberus-gaap:TradeNamesMember2022-01-012022-12-31
0001047335nhc:AcquisitionOfCarisMembernhc:CertificatesOfNeedAndLicensesMember2022-01-012022-12-31
0001047335nhc:DeferredTaxAssetsMember2019-12-31
0001047335nhc:LiabilityForUnrecognizedTaxBenefitsMember2019-12-31
0001047335nhc:LiabilityForInterestAndPenaltiesMember2019-12-31
0001047335nhc:TotalLiabilityMember2019-12-31
0001047335nhc:DeferredTaxAssetsMember2020-01-012020-12-31
0001047335nhc:LiabilityForUnrecognizedTaxBenefitsMember2020-01-012020-12-31
0001047335nhc:LiabilityForInterestAndPenaltiesMember2020-01-012020-12-31
0001047335nhc:TotalLiabilityMember2020-01-012020-12-31
0001047335nhc:DeferredTaxAssetsMember2020-12-31
0001047335nhc:LiabilityForUnrecognizedTaxBenefitsMember2020-12-31
0001047335nhc:LiabilityForInterestAndPenaltiesMember2020-12-31
0001047335nhc:TotalLiabilityMember2020-12-31
0001047335nhc:DeferredTaxAssetsMember2021-01-012021-12-31
0001047335nhc:LiabilityForUnrecognizedTaxBenefitsMember2021-01-012021-12-31
0001047335nhc:LiabilityForInterestAndPenaltiesMember2021-01-012021-12-31
0001047335nhc:TotalLiabilityMember2021-01-012021-12-31
0001047335nhc:DeferredTaxAssetsMember2021-12-31
0001047335nhc:LiabilityForUnrecognizedTaxBenefitsMember2021-12-31
0001047335nhc:LiabilityForInterestAndPenaltiesMember2021-12-31
0001047335nhc:TotalLiabilityMember2021-12-31
0001047335nhc:DeferredTaxAssetsMember2022-01-012022-12-31
0001047335nhc:LiabilityForUnrecognizedTaxBenefitsMember2022-01-012022-12-31
0001047335nhc:LiabilityForInterestAndPenaltiesMember2022-01-012022-12-31
0001047335nhc:TotalLiabilityMember2022-01-012022-12-31
0001047335nhc:DeferredTaxAssetsMember2022-12-31
0001047335nhc:LiabilityForUnrecognizedTaxBenefitsMember2022-12-31
0001047335nhc:LiabilityForInterestAndPenaltiesMember2022-12-31
0001047335nhc:TotalLiabilityMember2022-12-31
0001047335us-gaap:EmployeeStockOptionMember2022-01-012022-12-31
0001047335nhc:The2020EquityIncentivePlanMember2020-05-01
0001047335nhc:The2020EquityIncentivePlanMember2022-12-31
0001047335nhc:SalariesWagesAndBenefitsMember2022-01-012022-12-31
0001047335nhc:SalariesWagesAndBenefitsMember2021-01-012021-12-31
0001047335nhc:SalariesWagesAndBenefitsMember2020-01-012020-12-31
0001047335nhc:ExercisePriceRange1Member2022-12-31
0001047335nhc:ExercisePriceRange1Member2022-01-012022-12-31
0001047335nhc:ExercisePriceRange2Member2022-12-31
0001047335nhc:ExercisePriceRange2Member2022-01-012022-12-31
0001047335us-gaap:LineOfCreditMembernhc:NationalHealthCareMember2022-12-31
0001047335us-gaap:LineOfCreditMembernhc:NationalHealthCareMember2021-12-31
0001047335nhc:NationalMember2022-12-31
0001047335nhc:NationalMember2022-01-012022-12-31
0001047335nhc:NationalMember2021-01-012021-12-31
0001047335nhc:NationalMember2020-01-012020-12-31
0001047335nhc:NationalMember2021-12-31
0001047335nhc:NationalMemberus-gaap:CommonStockMember2022-12-31
0001047335nhc:NationalMemberus-gaap:CommonStockMember2021-12-31
0001047335nhc:NationalMemberus-gaap:CommonStockMember2020-12-31
0001047335us-gaap:VariableInterestEntityPrimaryBeneficiaryMember2022-12-31
0001047335us-gaap:VariableInterestEntityPrimaryBeneficiaryMember2010-12-31
0001047335us-gaap:VariableInterestEntityPrimaryBeneficiaryMembersrt:ConsolidationEliminationsMember2022-12-31
0001047335us-gaap:VariableInterestEntityPrimaryBeneficiaryMembersrt:ConsolidationEliminationsMember2021-12-31
0001047335us-gaap:VariableInterestEntityPrimaryBeneficiaryMemberus-gaap:LandBuildingsAndImprovementsMember2022-12-31
0001047335us-gaap:VariableInterestEntityPrimaryBeneficiaryMemberus-gaap:LandBuildingsAndImprovementsMember2021-12-31
0001047335nhc:OperationsTransferAgreementsForTransferOfSkilledNursingFacilitiesMember2022-09-012022-09-01
0001047335nhc:SevenSkilledNursingFacilitiesMembernhc:OperationsTransferAgreementsForTransferOfSkilledNursingFacilitiesMember2022-01-012022-12-31
0001047335nhc:SevenSkilledNursingFacilitiesMembernhc:OperationsTransferAgreementsForTransferOfSkilledNursingFacilitiesMember2021-01-012021-12-31
0001047335nhc:SevenSkilledNursingFacilitiesMembernhc:OperationsTransferAgreementsForTransferOfSkilledNursingFacilitiesMember2020-01-012020-12-31
0001047335nhc:AccruedRiskReservesMember2019-12-31
0001047335nhc:AccruedRiskReservesMember2020-01-012020-12-31
0001047335nhc:AccruedRiskReservesMember2020-12-31
0001047335nhc:AccruedRiskReservesMember2021-01-012021-12-31
0001047335nhc:AccruedRiskReservesMember2021-12-31
0001047335nhc:AccruedRiskReservesMember2022-01-012022-12-31
0001047335nhc:AccruedRiskReservesMember2022-12-31
0001047335nhc:COVID19Member2022-01-012022-12-31
Table of Contents
| UNITED STATES |
| SECURITIES AND EXCHANGE COMMISSION |
| WASHINGTON, D.C. 20549 |
| |
|
| FORM 10-K |
| (Mark One) | |
| ☒ ANNUAL REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES AND EXCHANGE ACT OF 1934 |
| For the fiscal year ended December 31, 2022 |
| OR |
| ☐ TRANSITION REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934 |
| For the transition period from __________ to _____________ |
| | |
| Commission File No. 001-13489 |
|
|
|
|
| (Exact name of registrant as specified in its Corporate Charter) |
| | |
| Delaware | 52-2057472 |
| (State of Incorporation) | (I.R.S. Employer Identification No.) |
| | |
| 100 E. Vine Street |
| Murfreesboro, Tennessee 37130 |
| (Address of principal executive offices) |
| Telephone Number: 615–890–2020 |
|
|
| Securities registered pursuant to Section 12(b) of the Act. |
| | |
| Title of Each Class | Trading Symbol(s) | Name of Each Exchange on which Registered |
| Shares of Common Stock | NHC | NYSE-American |
|
|
| Securities registered pursuant to Section 12(g) of the Act: None |
|
|
| Indicate by check mark if the registrant is a well–known seasoned issuer, as defined in Rule 405 of the Securities Act. Yes ☐ No ☒ |
| | |
| Indicate by check mark if the registrant is not required to file reports pursuant to Section 13 or Section 15(d) of the Act. Yes ☐ No ☒ |
| |
| Indicate by check mark whether the registrant (1) has filed all reports required to be filed by Section 13 or 15(d) of the Securities Exchange Act of 1934 during the preceding 12 months (or for such shorter period that the registrant was required to file such reports), and (2) has been subject to such filing requirements for the past 90 days: Yes ☒ No ☐ |
| | |
| Indicate by check mark whether the registrant has submitted electronically every Interactive Data File required to be submitted pursuant to Rule 405 of Regulation S–T (§232.405 of this chapter) during the preceding 12 months (or for such period that the registrant was required to submit such files). Yes ☒ No ☐ |
| | |
| Indicate by check mark whether the registrant is a large accelerated filer, an accelerated filer, a non–accelerated filer, a smaller reporting company, or an emerging growth company. See the definitions of “large accelerated filer,” “accelerated filer,” “smaller reporting company,” and “emerging growth company” in Rule 12b-2 of the Exchange Act. Large accelerated filer ☒ Accelerated filer ☐ Non–accelerated filer ☐ Smaller reporting company ☐ Emerging growth company ☐ |
| | |
| If an emerging growth company, indicate by checkmark if the registrant has elected not to use the extended transition period for complying with any new or revised financial accounting standards provided pursuant to Section 13(a) of the Exchange Act. ☐ |
| |
| Indicate by check mark whether the registrant has filed a report on and attestation to its management’s assessment of the effectiveness of its internal control over financial reporting under Section 404(b) of the Sarbanes-Oxley Act (15 U.S.C. 7262(b)) by the registered public accounting firm that prepared or issued its audit report. ☒ |
| |
| If securities are registered pursuant to Section 12(b) of the Act, indicate by check mark whether the financial statements of the registrant included in the filing reflect the correction of an error to previously issued financial statements. ☐ |
| |
| Indicate by check mark whether any of those error corrections are restatements that required a recovery analysis of incentive-based compensation received by any of the registrant's executive officers during the relevant recovery period pursuant to (§240.10D-1(b). ☐ |
| |
| Indicate by check mark whether the registrant is a shell company (as defined in Rule 12b–2 of the Exchange Act). Yes ☐ No ☒ |
| |
| The aggregate market value of Common Stock held by non–affiliates on June 30, 2022 (based on the closing price of such shares on the NYSE American) was approximately $719.7 million. For purposes of the foregoing calculation only, all directors, named executive officers and persons known to the Registrant to be holders of 5% or more of the Registrant’s Common Stock have been deemed affiliates of the Registrant. |
| The number of shares of Common Stock outstanding as of February 6, 2023 was 15,355,389 |
| Documents Incorporated by Reference |
| The following documents are incorporated by reference into Part III, Items 10, 11, 12, 13 and 14 of this Form 10–K: |
| The Registrant’s definitive proxy statement for its 2023 shareholder’s meeting. |
TABLE OF CONTENTS
PART 1
CAUTIONARY NOTE REGARDING FORWARD-LOOKING STATEMENTS
Statements in this annual filing that are not historical facts are forward-looking statements. NHC cautions investors that any forward-looking statements made involve risks and uncertainties and are not guarantees of future performance. Investors should also refer to the risks identified in "Part 1. Item 1A. Risk Factors" for a discussion of various risk factors of the Company and that are inherent in the health care industry. Given these risks and uncertainties, we can give no assurance that these forward-looking statements will, in fact, transpire and, therefore, caution investors not to place undue reliance on them. The risks included here are not exhaustive. All forward-looking statements represent NHC's best judgment as of the date of this filing.
PART 1
National HealthCare Corporation, which we also refer to as NHC or the Company, began business in 1971. Our principal business is the operation of skilled nursing facilities, assisted living facilities, independent living facilities, homecare and hospice agencies, and behavioral health hospitals. Our business activities include providing sub–acute and post–acute skilled nursing care, intermediate nursing care, rehabilitative care, memory and Alzheimer’s care, senior living services, home health care services, hospice services, and behavioral health services. In addition, we provide management services, accounting and financial services, as well as insurance services to third party operators of health care facilities. We also own the real estate of 13 healthcare properties and lease these properties to third party operators. We operate in 8 states and our operations are primarily located in the Southeastern and Midwestern parts of the United States.
Description of the Business
The following table summarizes our operations by ownership status as of December 31, 2022:
| |
|
Owned |
|
|
Leased |
|
|
Managed |
|
|
Total |
|
| Skilled Nursing Facilities |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Number of facilities |
|
|
27 |
|
|
|
32 |
|
|
|
9 |
|
|
|
68 |
|
| Percentage of total |
|
|
39.7% |
|
|
|
47.1% |
|
|
|
13.2% |
|
|
|
100.0% |
|
| Licensed beds |
|
|
3,460 |
|
|
|
4,221 |
|
|
|
1,045 |
|
|
|
8,726 |
|
| Percentage of total |
|
|
39.6% |
|
|
|
48.4% |
|
|
|
12.0% |
|
|
|
100.0% |
|
| |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Assisted Living Facilities |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Number of facilities |
|
|
13 |
|
|
|
7 |
|
|
|
3 |
|
|
|
23 |
|
| Percentage of total |
|
|
56.5% |
|
|
|
30.5% |
|
|
|
13.0% |
|
|
|
100.0% |
|
| Units |
|
|
964 |
|
|
|
174 |
|
|
|
43 |
|
|
|
1,181 |
|
| Percentage of total |
|
|
81.6% |
|
|
|
14.7% |
|
|
|
3.7% |
|
|
|
100.0% |
|
| |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Independent Living Facilities |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Number of facilities |
|
|
1 |
|
|
|
3 |
|
|
|
1 |
|
|
|
5 |
|
| Percentage of total |
|
|
20.0% |
|
|
|
60.0% |
|
|
|
20.0% |
|
|
|
100.0% |
|
| Retirement apartments |
|
|
93 |
|
|
|
245 |
|
|
|
137 |
|
|
|
475 |
|
| Percentage of total |
|
|
19.6% |
|
|
|
51.6% |
|
|
|
28.8% |
|
|
|
100.0% |
|
| |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Behavioral Health Hospitals |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Number of facilities |
|
|
3 |
|
|
|
– |
|
|
|
– |
|
|
|
3 |
|
| Percentage of total |
|
|
100.0% |
|
|
|
– |
|
|
|
– |
|
|
|
100.0% |
|
| Licensed beds |
|
|
96 |
|
|
|
– |
|
|
|
– |
|
|
|
96 |
|
| Percentage of total |
|
|
100.0% |
|
|
|
– |
|
|
|
– |
|
|
|
100.0% |
|
| |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Homecare Agencies |
|
|
35 |
|
|
|
– |
|
|
|
– |
|
|
|
35 |
|
| Hospice Agencies |
|
|
29 |
|
|
|
– |
|
|
|
– |
|
|
|
29 |
|
Net Patient Revenues. The services we provide include a comprehensive range of health care services. In fiscal 2022, 95.8% of our net operating revenues and grant income were derived from such health care services. Highlights of health care services activities during 2022 were as follows:
| |
● |
Skilled Nursing Facilities. The most significant portion of our business and the base for our other health care services is the operation of our skilled nursing facilities (“SNF’s”). In our facilities, experienced medical professionals provide medical services prescribed by physicians. Registered nurses, licensed practical nurses, and certified nursing assistants provide comprehensive, individualized nursing care 24 hours a day. In addition, our facilities provide licensed therapy services, quality nutrition services, social services, activities, and housekeeping and laundry services. Revenues from the 59 facilities we own or lease are reported as net patient revenues in our financial statements. Management fee income is recorded as other revenues from the nine facilities that we manage. We generally charge 6% of facility net operating revenues for our management services. |
| |
|
|
| |
|
The following table shows the occupancy rates for our owned and leased skilled nursing facilities: |
| |
|
Year Ended December 31, |
|
| |
|
2022 |
|
|
2021 |
|
|
2020 |
|
| Overall census |
|
|
83.8% |
|
|
|
80.6% |
|
|
|
83.6% |
|
| |
● |
Rehabilitative Services. Our licensed therapists provide physical, speech, respiratory and occupational therapy for patients recovering from strokes, heart attacks, orthopedic conditions, neurological illnesses, or other illnesses, injuries, or disabilities. We maintained a rehabilitation staff of over 1,200 highly trained, professional therapists in 2022. Most of our rehabilitative services are for patients in our owned and managed skilled nursing facilities. However, we also provide services to 68 additional health care providers. Our rates for these services are competitive with other market rates. |
| |
● |
Medical Specialty Units. All our skilled nursing facilities participate in the Medicare program, and we have expanded our range of offerings by the creation of facility–specific medical specialty units such as our memory care units and sub-acute nursing units. Our trained staff provides care for Alzheimer’s patients in early, middle and advanced stages of the disease. We provide specialized care and programs for persons with Alzheimer’s or related disorders in dedicated units within many of our skilled nursing facilities. Our specialized rehabilitation programs are designed to shorten or eliminate hospital stays and help to reduce the cost of quality health care. We develop individualized patient care plans to target appropriate medical and functional planning objectives with a primary goal where feasible for a return to home or a similar environment. |
| |
● |
Assisted Living Facilities. Our assisted living facilities provide personal care services and assistance with general activities of daily living such as dressing, bathing, meal preparation and medication management. We perform resident assessments to determine what services are desired or required and our qualified staff encourages residents to participate in a range of activities. In 2022, the rate of occupancy was 71.6% compared to 68.2% in 2021. Certificates of Need (“CONs”) are not required to build these projects in most states, and we believe overbuilding has occurred in some of our markets. |
| |
● |
Independent Living Facilities. Our independent living facilities offer specially designed residential units for the active and ambulatory elderly and provide various ancillary services for our residents, including restaurants, activity rooms and social areas. Charges for services are paid from private sources without assistance from governmental programs. Independent living facilities may be licensed and regulated in some states, but do not require the issuance of a CON such as is required for skilled nursing facilities. We have, in several cases, developed independent living facilities adjacent to our nursing facilities. These units are rented by the month; thus, these facilities offer an expansion of our continuum of care. We believe these independent living units offer a positive marketing aspect to all our senior care offerings and services. In 2022, the rate of occupancy was 89.0% compared to 88.1% in 2021. |
| |
|
|
| |
|
We have one independent living facility which is a "continuing care community", where the resident pays a substantial entrance fee and a monthly maintenance fee. The resident then receives a full range of services, including skilled nursing and home health, without additional charge. |
| |
● |
Behavioral Health Hospitals. Our comprehensive continuum of care includes behavioral health services to both adults and geriatric patients with psychiatric, emotional, and addictive disorders. Currently, we operate three behavioral hospitals for adult and geriatric patients who require inpatient hospitalization due to mental disorders, including cognitive illnesses. We also offer intensive outpatient programs with individualized treatment plans based on the patient's clinical needs. |
| |
● |
Homecare Agencies. Our home health agencies (“homecares”) assist those who wish to stay at home or in assisted living residences but still require some degree of medical care or assistance with daily activities. Registered and licensed practical nurses and therapy professionals provide skilled services such as infusion therapy, wound care and physical, occupational and speech therapies. Home health aides may assist with daily activities such as assistance with walking and getting in and out of bed, personal hygiene, medication assistance, light housekeeping and maintaining a safe environment. Under the Medicare reimbursement payment system, we receive a prospectively determined amount per patient per 30-day period of care. Under our managed care contracts, we may receive a period of care payment or be paid by a per-visit payment model. In 2022, we served an average census of 3,036 patients and provided 315,643 visits. |
| |
● |
Hospice Agencies. We provide hospice care through Caris Healthcare, L.P. (“Caris”), a wholly owned subsidiary of NHC. Caris specializes in providing hospice and palliative care to over 1,280 patients per day in 29 locations in Georgia, Missouri, South Carolina, Tennessee, and Virginia. Under the Medicare reimbursement payment system, Medicare pays a daily rate to cover the costs for providing services included in the patient care plan. Medicare makes daily payments based on 1 of 4 levels of hospice care. All hospice care and services offered to patients and their families must follow an individualized written plan of care that meets the patient’s needs. |
| |
● |
Pharmacy Operations. At December 31, 2022, we operated four regional pharmacy locations (two locations in Tennessee and one location each in South Carolina and Missouri). These pharmacies primarily service our patients that are in an inpatient setting using a central location to deliver pharmaceutical supplies. Our regional pharmacies bill Medicare Part D Prescription Drug Plans (PDPs) electronically and directly for inpatients who have selected a PDP. |
| |
● |
Institutional Special Needs Plan (“I-SNP”). Our I-SNP, which is called NHC Advantage, is a managed care insurance company that restricts enrollment to Medicare Advantage eligible individuals who, for 90 days or longer, have had or are expected to need the level of services provided in a skilled nursing facility. We believe the I-SNP benefits our patients by providing nurse practitioners and care-coordination teams that continue to enhance the patient-centered experience and our quality of patient care. The I-SNP receives a per member, per month premium from Medicare which covers the members same health care benefits as original Medicare, as well as additional benefits including preventive screenings and routine vision coverage. At December 31, 2022, the I-SNP operated in the states of Tennessee, Missouri, and South Carolina with approximately 1,100 members enrolled in the plan. |
Other Revenues. We generate revenues from management, accounting and financial services to third party operators of healthcare facilities, from insurance services to our managed healthcare facilities, and from rental income. In fiscal 2022, 4.2% of our net operating revenues and grant income were derived from such sources. The significant sources of our other revenues are described as follows:
| |
● |
Management, Accounting and Financial Services. We provide management services to skilled nursing facilities, assisted living facilities and independent living facilities operated by third party operators. We typically charge 6% of the managed centers’ net operating revenues as a fee for these services. Additionally, we provide accounting and financial services to other healthcare operators. As of December 31, 2022, we perform management services for thirteen healthcare facilities and accounting and financial services for 19 healthcare facilities. |
| |
● |
Insurance Services. NHC owns a Tennessee domiciled insurance company that provides workers’ compensation coverage to substantially all of NHC's owned and managed healthcare facilities. A second wholly owned insurance subsidiary is licensed in the Cayman Islands and provides general and professional liability coverage in substantially all of NHC’s owned and managed healthcare facilities. |
| |
● |
Rental Income. The healthcare properties currently owned and leased to third party operators include nine skilled nursing facilities and four assisted living communities. |
Government Stimulus Income. We received government stimulus funds as part of the Coronavirus Aid, Relief, and Economic Security Act (the "CARES ACT"). The CARES Act provided $2.2 trillion of economy-wide financial stimulus in the form of financial aid to individuals, businesses, nonprofits, states and municipalities. The CARES Act appropriated $178 billion to the Public Health and Social Services Emergency Fund, which is referred to as the Provider Relief Fund ("PRF"). The Company recorded $11,457,000, $63,360,000 and $47,505,000 of government stimulus income from the PRF for the years ended December 31, 2022, 2021, and 2020, respectively.
Non–Operating Income. We generate non–operating income from equity in earnings of unconsolidated investments, dividends and realized gains and losses on marketable securities, interest income, and other miscellaneous non–operating income.
Quality of Patient Care
CMS introduced the Five-Star Quality Rating System to help consumers, their families and caregivers compare skilled nursing facilities more easily. The Five-Star Quality Rating System gives each skilled nursing operation a rating ranging between one and five stars in various categories (five stars being the best). The Company has always strived for patient-centered care and quality outcomes as precursors to outstanding financial performance.
In July 2022, CMS launched its enhanced Five-Star Quality Rating System which integrates weekend staffing rates for nurses and information on annual turnover among nurses and administrators. The tables below summarize NHC's overall performance in these Five-Star ratings versus the skilled nursing industry as of December 31, 2022:
| |
|
NHC Ratings |
|
|
Industry Ratings |
|
| Total number of skilled nursing facilities, end of period |
|
|
68 |
|
|
|
|
|
| Number of 4 and 5-star rated skilled nursing facilities |
|
|
42 |
|
|
|
|
|
| Percentage of 4 and 5-star rated skilled nursing facilities |
|
|
62% |
|
|
|
37% |
|
| Average rating for all skilled nursing facilities, end of period |
|
|
3.8 |
|
|
|
2.9 |
|
Development and Growth
We are undertaking to expand our post–acute and senior health care operations while protecting our existing operations and markets. The following table lists our recent construction and purchase activities.
| Type of Operation |
|
Description |
|
Size |
|
Location |
|
Placed in Service |
| Skilled Nursing |
|
Acquisition |
|
166 beds |
|
Knoxville, TN |
|
February 2020 |
| Assisted Living |
|
Bed Addition |
|
20 beds |
|
Gallatin, TN |
|
September 2020 |
| Skilled Nursing |
|
Bed Addition |
|
30 beds |
|
Kingsport, TN |
|
December 2020 |
| Hospice |
|
Acquisition |
|
28 agencies |
|
Various |
|
June 2021 |
| Homecare |
|
New Agency |
|
1 agency |
|
Anderson, SC |
|
January 2022 |
| Hospice |
|
New Agency |
|
1 agency |
|
Tullahoma, TN |
|
March 2022 |
| Behavioral Health Hospital |
|
New Facility |
|
64 beds |
|
Knoxville, TN |
|
April 2022 |
| Behavioral Health Hospital |
|
New Facility |
|
16 beds |
|
St. Louis, MO |
|
June 2022 |
Business Segments
The Company has two reportable operating segments: (1) inpatient services, which includes the operation of skilled nursing facilities, assisted and independent living facilities, and behavioral health hospitals and (2) homecare and hospice services. The Company also reports an “all other” category that includes revenues from rental income, management and accounting services fees, insurance services, and costs of the corporate office. See Note 6 in the notes to the consolidated financial statements for further disclosure of the Company’s operating segments.
Customers and Sources of Revenues
No individual customer, or related group of customers, accounts for a significant portion of our revenues. We do not expect the loss of a single customer or group of related customers would have a material adverse effect.
Certain groups of patients receive funds to pay the cost of their care from a common source. The following table sets forth sources of net patient revenues for the periods indicated:
| |
|
Year Ended December 31, |
|
| Source |
|
2022 |
|
|
2021 |
|
|
2020 |
|
| Medicare |
|
|
37% |
|
|
|
36% |
|
|
|
33% |
|
| Managed Care |
|
|
10% |
|
|
|
11% |
|
|
|
11% |
|
| Medicaid |
|
|
28% |
|
|
|
29% |
|
|
|
31% |
|
| Private Pay and Other |
|
|
25% |
|
|
|
24% |
|
|
|
25% |
|
| Total |
|
|
100% |
|
|
|
100% |
|
|
|
100% |
|
We attempt to attract an increased percentage of Medicare and private pay patients by providing rehabilitative and other post–acute care services. These services are designed to speed the patient's recovery and allow the patient to return home as soon as it is practical.
Medicare is a health insurance program for the aged and certain other chronically disabled individuals operated by the federal government. Medicare covers skilled nursing services for beneficiaries who require nursing care and/or rehabilitation services following a discharge from an acute care hospital. For each eligible day a Medicare beneficiary is in a skilled nursing facility, Medicare pays the facility a daily payment, subject to adjustment for certain factors such as a wage index in the geographic area. The payment covers all services provided by the skilled nursing facility for the beneficiary that day, including room and board, nursing, therapy and drugs, as well as an estimate of capital–related costs to deliver those services.
Medicaid is a medical assistance program for the indigent, operated by individual states with the financial participation of the federal government. The states in which we operate primarily use a cost–based reimbursement system. Under cost–based reimbursement systems, the skilled nursing facility is reimbursed for the reasonable direct and indirect allowable costs it incurred in a base year in providing routine resident care services as defined by the program. Seniors who enter skilled nursing facilities as private pay patients can become eligible for Medicaid once they have substantially depleted their assets. Medicaid is generally the largest source of funding for most skilled nursing facilities.
Private pay, managed care, and other payment sources include commercial insurance, individual patient funds, managed care plans and the Veterans Administration. Although payment rates vary among these sources, market forces and costs largely determine these rates. Private paying patients, private insurance carriers and the Veterans Administration generally pay based on the center's charges or specifically negotiated contracts.
We contract with over 60 managed care organizations ("MCO's") and insurance carriers for the provision of healthcare services by our owned and managed healthcare facilities.
Government Regulation
General
Health care is an area of extensive regulatory oversight and frequent regulatory change. The federal government and the states in which we operate regulate various aspects of our business. These regulatory bodies, among other things, require us annually to license our skilled nursing facilities and other health care businesses. To operate skilled nursing facilities and provide health care services we must comply with federal, state and local laws relating to the delivery and adequacy of medical care, distribution of pharmaceuticals, equipment, personnel, operating policies, fire prevention, rate–setting, building codes and environmental protection. Changes in the laws or new interpretations of existing laws as applied to the skilled nursing facilities, home health and hospice, or other components of our health care businesses, may have a significant impact on our operations.
Governmental and other authorities periodically inspect our healthcare facilities and home health and hospice agencies to assure that we continue to comply with their various standards. We must pass these inspections to continue our licensing under state law, to obtain certification under the Medicare and Medicaid programs, and to continue our participation in the Veterans Administration program. We can only participate in other third–party programs if our facilities pass these inspections.
From time to time, we, like others in the health care industry, may receive notices from federal and state regulatory agencies alleging that we failed to comply with applicable standards. These notices may require us to take corrective action and may impose civil money penalties and/or other operating restrictions. If our skilled nursing facilities or home health and hospice agencies fail to comply with these directives or otherwise fail to comply substantially with licensure and certification laws, rules and regulations, we could lose our certification as a Medicare and Medicaid provider and/or lose our licenses.
Local and state health and social service agencies and other regulatory authorities specific to their location regulate, to varying degrees, our assisted living facilities. Although regulations and licensing requirements vary significantly from state to state, they typically address, among other things, personnel education, training and records; facility services, including administration of medication, assistance with supervision of medication management and limited nursing services; physical plant specifications; furnishing of resident units; food and housekeeping services; emergency evacuation plans; and resident rights and responsibilities. If assisted living facilities fail to comply with licensing requirements, these facilities could lose their licenses. Most states also subject assisted living facilities to state or local building codes, fire codes and food service licensure or certification requirements. In addition, the manner and extent to which the assisted living industry is regulated at federal and state levels are evolving.
In all states in which we operate, before a skilled nursing facility can make a capital expenditure exceeding certain specified amounts or construct any new skilled health care beds, approval of the state health care regulatory agency or agencies must be obtained, and a Certificate of Need issued. The appropriate state health planning agency must review the Certificate of Need according to state specific guidelines before a Certificate of Need can be issued. A Certificate of Need is generally issued for a specific maximum amount of expenditure and the project must be completed within a specific time period. There is no advance assurance that we will be able to obtain a Certificate of Need in any instance. In some states, approval is also necessary in order to purchase existing health care beds, although the purchaser is normally permitted to avoid a full-scale Certificate of Need application procedure by giving advance written notice of the acquisition and giving written assurance to the state regulatory agency that the change of ownership will not result in a change in the number of beds, services offered and, in some cases, reimbursement rates at the facility.
While there are currently no significant legislative proposals to eliminate Certificates of Need pertaining to skilled nursing care in the states in which we do business, deregulation in the Certificate of Need area would likely result in increased competition and could adversely affect occupancy rates and the supply of licensed and certified personnel.
A significant goal of the federal health care system is to transform the delivery of health care by holding providers accountable for the cost and quality of care provided, Medicare and many commercial third-party payors are implementing Accountable Care Organization ("ACO") models in which groups of providers share in the benefit and risk of providing care to an assigned group of individuals. Other reimbursement methodology reforms in which we are participating or expect to participate in include value–based purchasing, in which a portion of provider reimbursement is redistributed based on relative performance on designated economic, clinical quality, and patient satisfaction metrics. Also, CMS is implementing demonstration programs to bundle acute care and post–acute care reimbursement to hold providers accountable for costs across a broader continuum of care. These reimbursement methodologies and similar programs are likely to continue and expand, both in public and commercial health plans. Providers who respond successfully to these trends and can deliver quality care at lower costs are likely to benefit financially.
Patient Confidentiality
We are also subject to laws and regulations enacted to protect the confidentiality of patient health information. The U.S. Department of Health and Human Services ("HHS") has issued rules that govern our use and disclosure of protected health information. We have established policies and procedures to comply with HIPAA privacy and security requirements. We maintain a company-wide HIPAA compliance plan, that we believe complies with the HIPAA privacy and security regulations. The HIPAA privacy and security regulations have and will continue to impose significant costs to the Company in order to comply with these standards. Our operations are also subject to any federal or state privacy-related laws that are more restrictive than the privacy regulations issued under HIPAA. These laws vary and could impose additional penalties for privacy and security breaches.
Medicare and Medicaid Participation
All skilled nursing facilities, owned, leased or managed by us are certified to participate in Medicare. All but eight (seven owned and one managed) of our affiliated skilled nursing facilities participate in Medicaid. All our homecare and hospice agencies participate in the Medicare and Medicaid programs, with Medicare comprising the majority of their revenue. Our behavioral health hospitals also participate in the Medicare and Medicaid program.
During the fiscal years, we received payments from Medicare and, if participating, from Medicaid. We record as receivables the amounts we ultimately expect to receive under the Medicare and Medicaid programs and record into profit or loss any differences in amounts received at the time of interim or final settlements. There have not been any adjustments that have had a material adverse effect on the Company within the last three years.
Medicare Legislation and Regulations
Skilled Nursing Facilities
Medicare is uniform nationwide and reimburses skilled nursing facilities under a fixed payment methodology called the Skilled Nursing Facility Prospective Payment System ("SNF PPS"). The SNF PPS includes a new case-mix model called the Patient-Driven Payment Model (“PDPM”), which focuses on a resident’s condition and care needs, rather than the amount of care provided to determine reimbursement levels. PDPM utilizes clinically relevant factors for determining Medicare payment by using ICD-10 diagnosis codes and other patient characteristics as the basis for patient classification. PDPM utilizes five case-mix adjusted payment components: physical therapy (“PT”), occupational therapy (“OT”), speech language pathology (“SLP”), nursing and social services and non-therapy ancillary services (“NTA”). It also uses a sixth non-case mix component to cover utilization of skilled nursing facility (“SNF”) resources that do not vary depending on resident characteristics.
In July 2022, CMS released its final rule outlining fiscal year 2023 Medicare payment rates and policy changes for skilled nursing facilities, which began on October 1, 2022. The fiscal year 2023 rule provided for an approximate 2.7% increase, or $904 million, compared to 2022 levels. The net increase includes a 3.9% market-basket increase plus a 1.5% market basket forecast error adjustment, less a 0.3% productivity adjustment and a 2.3% decrease in the FY 2023 SNF PPS rates as a result of the recalibrated parity adjustment. The recalibrated parity adjustment is a total of 4.6% and is being phased in over the next two years (2.3% annually).
The Coronavirus Aid, Relief and Economic Security Act (the “CARES” Act) and other subsequent Congressional actions temporarily suspended Medicare sequestration beginning May 1, 2020 through March 31, 2022. The Medicare sequestration policy reduces fee-for-service Medicare payments by 2 percent. Effective April 1, 2022, sequestration was reinstated but only 1% was reduced from Medicare payments from April 1, 2022 through June 30, 2022. Beginning July 1, 2022, sequestration was increased back to the 2% reduction of Medicare payments for the remainder of 2022. The CARES Act extends the sequestration policy through 2030 in exchange for this temporary suspension.
Homecares
Medicare is uniform nationwide and reimburses homecare agencies under a Patient-Driven Groupings Model (“PDGM”). Under PDGM, Medicare provides homecare agencies with payments for each 30-day period of care provided to beneficiaries. If a beneficiary is still eligible for care after the end of the first 30-day payment period, a second 30-day payment period can begin. There are no limits to the number of periods of care a beneficiary who remains eligible for the home health benefit can receive. While payment for each 30-day period of care is adjusted to reflect the beneficiary’s health condition and needs, a special outlier provision exists to ensure appropriate payment for those beneficiaries that have the most expensive care needs. The payment under the Medicare program is also adjusted for certain variables.
In October 2022, CMS released its final rule outlining fiscal year 2023 Medicare payment rates. CMS projects payments to home health agencies in fiscal year 2023 will increase in aggregate by 0.7%, or $125 million. The increase reflects the effects of the home health payment update percentage of 4.0%, a permanent behavioral assumption adjustment resulting in a decrease of 3.5%, and an estimated 0.2% increase that reflects the effects of an update to the fixed-dollar loss ratio used in determining outlier payments.
Hospice
Medicare payment rates are calculated as daily rates for each of four levels of care we deliver. Rates are set based on specific levels of care, are adjusted by a wage index to reflect healthcare labor costs across the country and are established annually through federal legislation. The following are the four levels of care provided under the hospice benefit:
| |
● |
Routine Home Care. Care that is not classified under any of the other levels of care, such as the work of nurses, social workers or home health aides. |
| |
● |
General Inpatient Care. Pain control or acute or chronic symptom management that cannot be managed in a setting other than an inpatient Medicare-certified facility, such as a hospital, skilled nursing facility or hospice inpatient facility. |
| |
● |
Continuous Home Care. Care for patients experiencing a medical crisis that requires nursing services to achieve palliation and symptom control if the agency provides a minimum of eight hours of care within a 24-hour period. |
| |
● |
Inpatient Respite Care. Short-term, inpatient care to give temporary relief to the caregiver who regularly provides care to the patient. |
Medicare payments are subject to two fixed annual caps, which are assessed on a provider number basis, and are broken into an inpatient cap amount and an overall payment cap. These cap amounts are calculated and published by the Medicare fiscal intermediary on an annual basis.
In July 2022, CMS released its final rule outlining fiscal year 2023 Medicare payment rates. CMS issued a rate increase of 3.8%, or $825 million, effective October 1, 2022. The increase is the result of a 4.1% inpatient hospital market basket increase reduced by a 0.3% productivity adjustment. The FY2023 hospice payment update also includes an update to the statutory aggregate cap amount, which limits the overall payments per patient that are made annually. The cap amount for FY2023 is $32,487.
Medicaid Legislation and Regulations
Skilled Nursing Facilities
State Medicaid plans subject to budget constraints are of particular concern to us. Changes in federal funding coupled with state budget problems and Medicaid expansion under the Affordable Care Act have produced an uncertain environment. Some states will not keep pace with post-acute healthcare inflation. States are currently under pressure to pursue other alternatives to skilled nursing care such as community and home–based services.
Medicaid programs are funded jointly by the federal government and the states and are administered by states under approved plans. Most state Medicaid payments are made under a prospective payment system or under programs which negotiate payment levels with individual providers. Some states use, or have applied to use, waivers granted by CMS to implement expansion, impose different eligibility or enrollment restrictions, or otherwise implement programs that vary from federal standards.
Effective July 1, 2022 and for the fiscal year 2023, the state of Tennessee implemented specific individual nursing facility increases. We estimate the resulting increase in revenue for the 2023 fiscal year will be approximately $3,200,000 annually, or $800,000 per quarter.
Effective October 1, 2022 and for the fiscal year 2023, the state of South Carolina implemented specific individual nursing facility increases. We estimate the resulting increase in revenue for the 2023 fiscal year will be approximately $3,735,000 annually, or $934,000 per quarter.
We have also received from many of the states in which we operate a supplemental Medicaid payment to help mitigate the incremental costs resulting from the COVID-19 public health emergency. For the years ended December 31, 2022, 2021 and 2020, we have recorded $19,442,000, $20,482,000 and $26,179,000, respectively, due to these supplemental Medicaid payments. We have recorded these payments in net patient revenues in our consolidated statements of operations.
Competition
In most of the communities in which we operate health care facilities, we compete with other health care facilities in the area. There are hundreds of operators of post-acute healthcare services in each of these states and no single operator, including us, dominates any of the markets, except for some small rural markets which might have limited competition. In competing for patients and staff, we depend upon referrals from acute care hospitals, physicians, residential care facilities, church groups and other community service organizations. The reputation in the community and the physical appearance of our facilities are important in obtaining patients since members of the patient’s family generally participate to a greater extent in selecting skilled nursing facilities than in selecting an acute care hospital. We believe that by providing and emphasizing rehabilitative, as well as patient-centered healthcare services, we can broaden our patient base and to differentiate our operations from competing operations.
As we continue to expand into all areas of senior health care, we monitor proposed or existing competing operations. Our development goal is to link our skilled nursing facilities with our senior living communities, home health and hospice operations, and behavioral health hospitals; therefore, obtaining a competitive advantage for our operations.
Human Capital
Employees
As of December 31, 2022, we had 12,355 full-time and part-time employees (“partners”) through our Administrative Services Contractor (National Health Corporation). None of our partners were represented by a collective bargaining agreement. We believe relations with our partners are good. Our partners are guided by NHC’s Code of Conduct, and they take pride in their work. The Company’s partners appreciate different perspectives and embrace the opportunity to work with those of diverse backgrounds.
Total Rewards
To attract and retain top talent, we believe we must offer and maintain competitive total rewards for our partners. These rewards include not only wages and salaries, but also health, welfare, and retirement benefits. Our partners accrue earned time off (“ETO”) with the flexibility to use this time at their discretion. We offer comprehensive health insurance coverage to all eligible partners as well as a partner and family sick time program which allows partners to accrue paid sick time based on hours worked and to use that time for themselves or family members in need of care. We offer a 401(k) plan which includes matching company contributions. Also, to foster a stronger sense of ownership, we offer an Employee Stock Purchase Plan where partners may purchase company stock through payroll deduction.
We face competition in employing and retaining nurses, technicians, aides, and other high-quality professional and non–professional employees. To enhance our competitive position, we offer a robust educational tuition reimbursement program, an American Dietetic Association approved internship program, specialty designed nurse aide training classes, and there is financial scholarship aid available for various health care vocation programs.
We also conduct an "Administrator in Training" course, which is 24 months in duration, for the professional training of skilled nursing facility administrators. Presently, we have three (two male and one female) full–time individuals in this program. All six of our regional vice presidents and 50 of our 68 health care center administrators are graduates of this program.
We regularly utilize third-party consultants to conduct anonymous surveys to seek feedback from our partners on a variety of topics, including but not limited to, confidence in company leadership, competitiveness of our compensation and benefits package, career growth opportunities and improvements on how we can continue to make our company an employer of choice. The results are shared with our partners and reviewed by senior leadership, who analyze areas of progress or deterioration and prioritize actions and activities in response to this feedback to drive meaningful improvements in partner engagement.
Health and Safety
The health and safety of our partners is our highest priority. We focus on safety training in order to maintain a safe work environment and minimize work-related injury. When the pandemic began, we ensured and continue to ensure that our partners have access to masks, thermometers, protective gloves, sanitizing supplies, and all personal protective equipment needed in order to protect themselves. We closely followed the recommendations of the World Health Organization, the U.S. Centers for Disease Control and local governments, and we took action to ensure our partners were safe. Some of the preventative measure we have implemented included:
| |
● |
increased hygiene, cleaning and sanitizing procedures at all locations; |
| |
● |
provided additional personal protective equipment to partners; |
| |
● |
restricted travel and encouraged quarantine upon return; |
| |
● |
encouraged employees to take time off for illness; |
| |
● |
established strict protocols and screening for outside guests; and |
| |
● |
enabled partners to work from home where possible. |
Community
We have a long and proud history of investing in the communities where we live and work. Through the National Health Foundation (the “Foundation”) and The Foundation for Geriatric Education (“TFGE”) we give back by providing grants to nonprofits and providing tuition reimbursement to partners to further their education in the field of geriatrics. We also have a Compassion Fund which is used to help support partners in times of need. Many of our partners make a positive impact in the communities in which they live by donating their time and talent by volunteering and serving on boards of charitable organizations.
Environmental Sustainability
We are working diligently to minimize our effect on the environment by conserving energy and protecting our natural resources. We are focusing on being more energy efficient and reducing our water use and wastewater discharges while continuing to provide a healthy environment for our patients, partners and visitors. We are committed to adhering to applicable federal, state and local environmental regulations. Our goal is to minimize environmental risks to our patients and in the communities which we operate.
Through recycling programs, we are working to reduce the amount of waste sent to landfills. Our electronic waste is recycled through a zero-landfill recycling company.
Available Information
The Company's Annual Reports on Form 10-K, Quarterly Reports on Form 10-Q and Current Reports on Form 8-K, and amendments to those reports filed or furnished pursuant to Section 13(a) or 15(d) of the Securities Exchange Act of 1934, are available free of charge at www.nhccare.com, as soon as reasonably practicable after the reports are electronically filed or furnished with the U.S. Securities and Exchange Commission ("SEC"). The SEC maintains a website that contains these reports as well as proxy statements and other information regarding issuers that file electronically. The SEC's website is at www.sec.gov. NHC's website and its content are not deemed incorporated by reference into this report.
You should carefully consider the risk factors set forth below, as well as the other information contained in this Annual Report on Form 10–K. These risk factors should be considered in connection with evaluating the forward–looking statements contained in this Annual Report on Form 10–K, because these factors could cause the actual results and conditions to differ materially from those projected in forward–looking statements. The risks described below are not the only risks facing us. Additional risks and uncertainties that are not currently known to us or that we currently deem to be immaterial may also materially and adversely affect our business operations. Any of the following risks could materially adversely affect our business, financial condition or results of operations and cash flows.
Risks Relating to Our Operations
COVID-19 and other pandemics, epidemics, or outbreaks of a contagious illness may adversely affect our operating results, cash flows and financial condition. The COVID-19 pandemic has had a negative impact and is expected to continue to have a negative impact on our business and results of operations. Although vaccines for the COVID-19 virus are widely available in the United States, COVID-19 cases remain high in some areas. According to the Centers for Disease Control and Prevention, older adults and people with certain underlying medical conditions are at higher risk for serious illness and death from COVID-19.
COVID-19 and other pandemics, epidemics, or outbreaks of a contagious illness, and similar events, may cause harm to us, our partners (employees), our patients, our vendors and supply chain partners, and financial institutions, which could have a material adverse effect on our results of operations, financial condition and cash flows. The COVID-19 impacts may include, but would not be limited to:
| |
● |
Disruption to operations due to the unavailability of partners due to illness, quarantines, risk of illness, travel restrictions or factors that limit our existing or potential workforce. |
| |
● |
Increased costs and staffing requirements related to additional CDC protocols, federal and state workforce protection and related isolation procedures, including obligations to test patients and staff for COVID-19. |
| |
● |
Decreased availability and increased cost of supplies due to increased demand around essential personal protective equipment (“PPE”), sanitizers and cleaning supplies including disinfecting agents, and food and food-related products due to increased global demand and disruptions along the global supply chains of these manufactures and distributors. |
| |
● |
Decreased census across all our operations, which could negatively impact our operating cash flows and financial condition. |
| |
● |
Elevated partner turnover which may increase payroll expense, increase third party agency nurse staffing, and recruiting-related expenses. |
| |
● |
Increased risk of litigation and related liabilities arising in connection with patient or partner illness, hospitalization and/or death. |
| |
● |
Significant disruption of the global financial markets, which could have a negative impact on our ability to access capital in the future. |
The further spread of COVID-19, and the measures taken by federal and state governments and local health authorities intended to limit the spread of the virus, could impact the resources required to carry out our business as usual and may have a material adverse effect on our results of operations, financial condition and cash flows. The extent to which the COVID-19 pandemic will impact our business and our financial results will depend on future developments, which are highly uncertain and cannot be predicted. Such developments may include the ongoing geographic spread of the virus, the severity and the duration of the pandemic, the timing, availability and effectiveness of medical treatments and vaccines (including additional doses of vaccines), the impact of any mutations of the virus, and the type, duration and efficacy of actions that may be taken by various governmental authorities to contain the virus or treat its impact, among others. Any of these developments, individually or in aggregate, could materially impact our business and our financial results and condition.
We depend on reimbursement from Medicare, Medicaid and other third–party payors, and reimbursement rates from such payors may be reduced. We derive a substantial portion of our revenue from third–party payors, including the Medicare and Medicaid programs. Third–party payor programs are highly regulated and are subject to frequent and substantial changes. Changes in the reimbursement rate or methods of payment from third–party payors, including the Medicare and Medicaid programs, or the implementation of other measures to reduce reimbursements for our services has in the past, and could in the future, result in a substantial reduction in our revenues and operating margins. For example, the Budget Control Act of 2011 requires automatic spending reductions to reduce the federal deficit, imposing Medicare spending reductions of up to 2% per fiscal year, with a uniform percentage across all Medicare programs. CMS began imposing a 2% reduction on Medicare claims in 2013, and these reductions have been extended through 2030. The CARES Act and related legislation temporarily suspended this 2% reduction through March 31, 2022, and reduced the sequestration adjustment from 2% to 1% from April 1 through June 30, 2022. The full 2% reduction took effect July 1, 2022.
Net revenue realizable under third–party payor agreements can change after examination and retroactive adjustment by payors during the claims settlement processes or as a result of post–payment audits. Payors may disallow requests for reimbursement based on determinations that certain costs are not reimbursable or reasonable because additional documentation is necessary or because certain services were not covered or were not reasonable and medically necessary.
Our hospice agencies are subject to two payment caps that limit Medicare reimbursement each federal fiscal year, an inpatient cap and an aggregate cap. The inpatient cap limits the number of days of inpatient care to no more than 20% of total patient care days. The aggregate cap limits the total Medicare reimbursement that a hospice may receive based on an annual per-beneficiary cap amount and the number of Medicare patients served. If payments received by any one of our hospice provider numbers exceeds the inpatient or aggregate caps, we are required to reimburse Medicare for payments received in excess of the caps, which could have a material adverse effect on our business.
We cannot assure you that adequate reimbursement levels will continue to be available for the services provided by us. Further limits on the scope of services reimbursed and on reimbursement rates could have a material adverse effect on our liquidity, financial condition and results of operations. It is possible that the effects of further refinements to payment systems that result in lower payments to us or cuts in state Medicaid funding could have a material adverse effect on our results of operations. See Item 1, "Business – Government Regulation" and "Business - Medicare Legislation and Regulations".
The industry trend toward value-based purchasing may negatively impact our revenues. There continues to be a growing trend in the healthcare industry among both government and commercial payors toward value-based purchasing of healthcare services. Value-based purchasing programs emphasize quality and efficiency of services, rather than volume of services. For example, CMS reimburses SNF providers using the PDPM, a payment methodology that classifies patients into payment groups based on clinical factors using diagnosis codes rather than by volume of services. In addition, CMS requires SNFs, home health agencies and hospices to report quality data in order to receive full reimbursement. Failure to report quality data or poor performance may negatively impact the amount of reimbursement received. CMS publishes quality measure data online through its Care Compare website, to allow the public to search and compare data for Medicare-certified providers.
Under the SNF Value-Based Purchasing Program, CMS reduces SNF Medicare payments by 2 percentage points and redistributes the majority of these funds as incentive payments based on SNF quality measure performance. In January 2022, CMS began implementing a nationwide expansion of the Home Health Value-Based Purchasing (“HHVBP) Model. Under the model, home health agencies will receive increases or decreases to their Medicare fee-for-service payments of up to 5%, based on performance against specific quality measures relative to the performance of other providers. Data collected in each performance year will impact Medicare payments two years later. Calendar year 2023 is the first performance year under the expanded HHVBP Model that will affect payments.
Other initiatives aimed at improving the cost of care include alternative payment models, such as ACOs and bundled payment arrangements. Medicare and many commercial third-party payors are implementing ACO models, in which groups of providers share in the benefit and risk of providing care to an assigned group of individuals at a lower cost. In addition, CMS is implementing programs to bundle acute care and post-acute care reimbursement to hold providers accountable for costs across a broader continuum of care. In October 2021, the CMS Innovation Center released an outline of its strategy for the next decade, noting the need to accelerate the movement to value-based care and drive broader system transformation. By 2030, the CMS Innovation Center aims to have all fee-for-service Medicare beneficiaries and the vast majority of Medicaid beneficiaries in an accountable care relationship with providers who are responsible for quality and total medical costs. The CMS Innovation Center signaled its intent to streamline its payment models and to increase provider participation through implementation of more mandatory models.
These reimbursement methodologies and other value-based care initiatives are likely to continue and expand, at both the federal and state levels and in public and commercial health plans. It is unclear whether alternative payment models will successfully coordinate care and reduce costs or whether they will decrease overall reimbursement. As a result, it is difficult to predict how the trend toward value-based purchasing will ultimately affect our business. If we fail to meet or exceed quality performance standards under any applicable value-based purchasing program, perform at a level below the outcomes demonstrated by our competitors, or otherwise fail to effectively provide or coordinate the efficient delivery of quality health care services, our reputation in the industry may be negatively impacted, we may receive reduced reimbursement amounts, and we may owe repayments to payors, causing our revenues to decline. Failure to respond successfully to value-based purchasing trends could negatively impact our business, results of operations and/or financial condition.
By undertaking to provide management services, advisory services, and/or financial services to other entities, we become at least partially responsible for meeting the regulatory requirements of those entities. We provide management and/or financial services to skilled nursing facilities, assisting living facilities and independent living facilities owned by third parties. The "Risk Factors" contained herein as applying to us may in many instances apply equally to these other entities for which we provide services. We have in the past and may in the future be subject to claims from the entities to which we provide management, advisory or financial services, or to the claims of third parties to those entities. Any adverse determination in any legal proceeding regarding such claims could have a material adverse effect on our business, our results of operation, our financial condition and cash flows.
We provide management services to skilled nursing facilities and other healthcare facilities under terms whereby the payments for our services are subject to subordination to other expenditures of the healthcare facility. Furthermore, there are certain third parties with whom we have contracted to provide services and which we have determined, based on insufficient historical collections and the lack of expected future collections, that the service revenue realization is uncertain. We may, therefore, make expenditures related to the provision of services for which we are not paid.
The cost to replace or retain qualified nurses, health care professionals and other key personnel may adversely affect our financial performance, and we may not be able to comply with certain states’ staffing requirements. We could experience significant increases in our operating costs due to shortages in qualified nurses, health care professionals and other key personnel. The market for these key personnel is highly competitive. We, like other health care providers, have experienced difficulties in attracting and retaining qualified personnel, especially facility administrators, nurses, certified nurses' aides and other important health care providers. There is currently a shortage of nurses, and trends indicate this shortage will continue or worsen in the future. The difficulty our skilled nursing facilities are experiencing in hiring and retaining qualified personnel has increased our average wage rate. We may continue to experience increases in our labor costs due to higher wages and greater benefits required to attract and retain qualified health care personnel. Our ability to control labor costs will significantly affect our future operating results. Additionally, if we fail to attract and retain qualified and skilled personnel, our ability to conduct our business operations effectively could be harmed.
Certain states in which we operate skilled nursing facilities have adopted minimum staffing standards and additional states may also establish similar requirements in the future. Our ability to satisfy these requirements will depend upon our ability to attract and retain qualified nurses, certified nurses' assistants, and other staff. Failure to comply with these requirements may result in the imposition of fines or other sanctions. If states do not appropriate sufficient additional funds (through Medicaid program appropriations or otherwise) to pay for any additional operating costs resulting from minimum staffing requirements, our profitability may be adversely affected.
The staffing level required to receive a 5-star rating in the CMS Nursing Home Five Star Quality Rating System is determined based on analysis of the relationship between staffing levels and measures of nursing home quality. CMS places a strong emphasis on registered nurse (“RN”) staffing. The overall and RN staffing ratings are set to one star for nursing homes that report four or more days in the quarter with no RN on-site. Finally, staffing ratings are not suppressed for nursing homes that have five or more days with residents and no nurse staffing hours reported. CMS posts information on nursing home staffing measures on the Care Compare website including staff turnover rates and weekend staffing levels. This new data has been incorporated into the Nursing Home Five Star Quality Rating System.
Although we currently have no collective bargaining agreements with unions at our facilities, there is no assurance this will continue to be the case. If any of our facilities enter into collective bargaining agreements with unions, we could experience or incur additional administrative expenses associated with union representation of our employees.
Our senior management team has extensive experience in the healthcare industry. We believe they have been instrumental in guiding our business, instituting valuable performance and quality monitoring, and driving innovation. Accordingly, our future performance is substantially dependent upon the continued services of our senior management team. The loss of the services of any of these persons could have a material adverse effect upon us.
Disasters and similar events, which may increase as a result of climate change, may seriously harm our business. Natural and man–made disasters and similar events, including terrorist attacks and acts of nature such as hurricanes, tornadoes, earthquakes and wildfires, may cause damage or disruption to us, our employees and our facilities, which could have an adverse impact on our patients and our business. In order to provide care for our patients, we are dependent on consistent and reliable delivery of food, pharmaceuticals, utilities and other goods to our facilities, and the availability of employees to provide services at our facilities. If the delivery of goods or the ability of employees to reach our facilities were interrupted in any material respect due to a natural disaster or other reasons, it would have a significant impact on our facilities and our business. Furthermore, the impact, or impending threat, of a natural disaster has in the past and may in the future require that we evacuate one or more facilities, which would be costly and would involve risks, including potentially fatal risks, for the patients. The impact of disasters and similar events is inherently uncertain. Such events could harm our patients and employees, severely damage or destroy one or more of our facilities, harm our business, reputation and financial performance, or otherwise cause our business to suffer in ways that we currently cannot predict.
Significant changes in the climate may occur in areas where our facilities are located and we may experience more frequent extreme weather events which may result in physical damage to or a decrease in demand for our facilities located in these areas or affected by these conditions. In addition, changes in federal and state legislation and regulation on climate change could result in increased capital expenditures to improve the energy efficiency of our facilities without a corresponding increase in revenue. Climate change may also have indirect effects on our business by increasing the cost of (or making unavailable) property insurance on terms we find acceptable. Should the impact of climate change be material in nature, including destruction of our facilities, or occur for lengthy periods of time, our financial condition or results of operations may be adversely affected.
Future acquisitions or new developments may be difficult to complete, use significant resources, or be unsuccessful and could expose us to unforeseen liabilities. We may selectively pursue acquisitions or new developments in our target markets. Acquisitions and new developments may involve significant cash expenditures, debt incurrence, capital expenditures, additional operating losses, amortization of the intangible assets of acquired companies, dilutive issuances of equity securities and other expenses that could have a material adverse effect on our financial condition and results of operations. Acquisitions also involve numerous other risks, including difficulties integrating acquired operations, personnel and information systems, diversion of management's time from existing operations, potential losses of key employees or customers of acquired companies, assumptions of significant liabilities, exposure to unforeseen liabilities of acquired companies and increases in our indebtedness.
We cannot assure that we will succeed in obtaining financing for any acquisitions at a reasonable cost or that any financing will not contain restrictive covenants that limit our operating flexibility. We also may be unable to operate acquired facilities profitably or succeed in achieving improvements in their financial performance.
We also may face competition in acquiring any facilities. Our competitors may acquire or seek to acquire many of the facilities that would be suitable acquisition candidates for us. This could limit our ability to grow by acquisitions or increase the cost of our acquisitions.
In addition, federal and state regulation may adversely impact our ability to complete acquisitions or pursue new developments. For example, a Medicare regulation known as the “36 Month Rule” prohibits the buyer of a Medicare-certified home health agency from assuming the Medicare billing privileges of an acquired agency if the acquired agency either enrolled in Medicare or underwent a change in majority ownership fewer than 36 months prior to the acquisition, subject to certain exceptions. Instead, the buyer must enroll the acquired home health agency as a new provider with Medicare. The 36 Month Rule may increase competition for acquisition targets that are not subject to the rule and may cause significant Medicare billing delays for purchases of home health agencies that are subject to the rule. In addition, our ability to expand operations in a state depends on our ability to obtain necessary state licenses to operate and, where required, certificate of need approval. States may limit the number of licenses they issue. The failure to obtain any required license or certificate of need could impair our ability to operate or expand our business.
Upkeep of healthcare properties is capital intensive, requiring us to continually direct financial resources to the maintenance and enhancement of our physical plant and equipment. As of December 31, 2022, we leased or owned 59 skilled nursing facilities, 20 assisted living facilities, and four independent living facilities. Our ability to maintain and enhance our physical plant and equipment in a suitable condition to meet regulatory standards, operate efficiently and remain competitive in our markets requires us to commit a substantial portion of our free cash flow to continued investment in our physical plant and equipment. Certain of our competitors may operate centers that are not as old as our centers, or may appear more modernized than our centers, and therefore may be more attractive to prospective customers. In addition, the cost to replace our existing centers through acquisition or construction is substantially higher than the carrying value of our centers. We are undertaking a process to allocate more aggressive capital spending within our owned and leased facilities in an effort to address issues that arise in connection with an aging physical plant.
If factors, including factors indicated in these "Risk Factors" and other factors beyond our control render us unable to direct the necessary financial and human resources to the maintenance, upgrade and modernization of our physical plant and equipment, our business, results of operations, financial condition and cash flow could be adversely impacted.
We are defendants in significant legal actions, which are commonplace in our industry, and which could subject us to increased operating costs and substantial uninsured liabilities, which would materially and adversely affect our liquidity and financial condition. As is typical in the health care industry, we are subject to claims that our services have resulted in resident injury or other adverse effects. We, like our industry peers, have experienced an increasing trend in the frequency and severity of professional liability and workers’ compensation claims and litigation asserted against us. In some states in which we have significant operations, insurance coverage for the risk of punitive damages arising from professional liability claims and/or litigation may not, in certain cases, be available due to state law prohibitions or limitations of availability. We cannot assure you that we will not be liable for punitive damage awards that are either not covered or are in excess of our insurance policy limits. We also believe that there have been, and will continue to be, governmental investigations of long–term care providers, particularly in the area of Medicare/Medicaid false claims, as well as an increase in enforcement actions resulting from these investigations. Insurance is not available to cover such losses. Any adverse determination in a legal proceeding or governmental investigation, whether currently asserted or arising in the future, could have a material adverse effect on our financial condition.
Due to the rising cost and limited availability of professional liability and workers’ compensation insurance, we are largely self–insured on all of these programs and as a result, there is no limit on the maximum number of claims or amount for which we or our insurance subsidiaries can be liable in any policy period. Although we base our loss estimates on independent actuarial analyses using the information we have to date, the amount of the losses could exceed our estimates. In the event our actual liability exceeds our estimates for any given period, our results of operations and financial condition could be materially adversely impacted. In addition, our insurance coverage might not cover all claims made against us. If we are unable to maintain our current insurance coverage, if judgments are obtained in excess of the coverage we maintain, if we are required to pay uninsured punitive damages, or if the number of claims settled within the self–insured retention currently in place significantly increases, we could be exposed to substantial additional liabilities. We cannot assure you that the claims we pay under our self–insurance programs will not exceed the reserves we have set aside to pay claims. The number of claims within the self–insured retention may increase.
If we fail to compete effectively with other health care providers, our revenues and profitability may decline. The health care services industry is highly competitive. Our skilled nursing facilities, assisted living facilities, independent living facilities, hospices, home care services and other operations compete on a local and regional basis with other nursing centers, health care providers, and senior living service providers that provide services similar to those we offer. Some of our competitors' facilities are located in newer buildings and may offer services not provided by us or are operated by entities having greater financial and other resources than us. Certain of our competitors are operated by not-for-profit, non-taxpaying or governmental agencies that can finance capital expenditures on a tax-exempt basis and that receive funds and charitable contributions unavailable to us. Consolidations of not-for-profit entities may intensify this competitive pressure. Many competing general acute care hospitals are larger and more established than our facilities.
There is also increasing consolidation in the third-party payer industry, including vertical integration efforts among third-party payers and healthcare providers. Healthcare industry participants are increasingly implementing physician alignment strategies, such as employing physicians, acquiring physician practice groups and participating in ACOs or other clinical integration models. Other industry participants, such as large employer groups and their affiliates, may intensify competitive pressure and affect the industry in ways that are difficult to predict. Trends toward clinical transparency and value-based purchasing may impact our competitive position and patient volumes.
Our facilities compete based on factors such as our reputation for quality care; the commitment and expertise of our staff; the quality and comprehensiveness of our treatment programs; the physical appearance, location and condition of our facilities and to a limited extent, the charges for services. In addition, we compete with other health care providers for customer referrals from hospitals and other providers. As a result, a failure to compete effectively with respect to referrals may have an adverse impact on our business. We cannot assure that increased competition in the future will not adversely affect our financial condition and results of operations.
Possible changes in the case mix of patients and payor mix may significantly affect our profitability. The sources and amounts of our patient revenues will be determined by a number of factors, including licensed bed capacity and occupancy rates of our facilities, the mix of patients and the rates of reimbursement among payors. Changes in the case mix of the patients as well as payor mix among private pay, Medicare and Medicaid will significantly affect our profitability. Particularly, any significant increase in our Medicaid population could have a material adverse effect on our financial position, results of operations and cash flow, especially if states operating these programs continue to limit, or more aggressively seek limits on, reimbursement rates or service levels.
Private third–party payors continue to try to reduce health care costs. Private third–party payors are continuing their efforts to control health care costs through direct contracts with health care providers, increased utilization review and greater enrollment in managed care programs and preferred provider organizations, among other strategies. These private payors increasingly are demanding discounted fee structures and the assumption by health care providers of all or a portion of the financial risk. The ability of private payors to control healthcare costs may be enhanced by the increasing consolidation of insurance companies and the vertical integration of health insurers with healthcare providers. We could be adversely affected by the continuing efforts of private third–party payors to limit the amount of reimbursement we receive for health care services. We cannot assure you that reimbursement under private third–party payor programs will remain at levels comparable to present levels or will be sufficient to cover the costs allocable to patients eligible for reimbursement pursuant to such programs. Future changes in the reimbursement rates or methods of private or third–party payors or the implementation of other measures to reduce reimbursement for our services could result in a substantial reduction in our net operating revenues. As a result of competitive pressures, our ability to maintain operating margins through price increases to private patients is limited.
In addition, the failure to obtain, renew, or retain payor agreements with favorable contract terms may negatively impact our results of operations and/or revenue. Our ability to contract with payors depends on our quality of service and reputation, as well as other factors of which we may have little or no control, such as state appropriations and changes in provider eligibility requirements.
We are permitted to incur substantially more debt, which could further exacerbate the risks described above. We and our subsidiaries may be able to incur substantial indebtedness in the future. If debt is added, the related risks that we now face could intensify.
Risks Related to Government Regulation
We conduct business in a heavily regulated industry, and changes in, or violations of regulations may result in increased costs or sanctions that reduce our revenue and profitability. In the ordinary course of our business, we are regularly subject to inquiries, investigations and audits by federal and state agencies to determine whether we are in compliance with regulations governing the operation of, and reimbursement for, skilled nursing facilities and nursing homes, assisted living and independent living facilities, hospice, home health agencies and our other operating areas. These regulations include those relating to licensure, certification and enrollment with government programs, conduct of operations, ownership of facilities, construction of new and additions to existing facilities, allowable costs, adequacy and quality of services, qualifications and training of personnel, communications with patients and consumers, billing and coding for services, adequacy and manner of documentation for services provided, minimum direct care spending ratios, services and prices for services, and pharmaceuticals and controlled substances. Various laws, including federal and state anti–kickback and anti–fraud statutes, prohibit certain business practices and relationships that might affect the provision and cost of health care services reimbursable under federal and/or state health care programs such as Medicare and Medicaid, including the payment or receipt of remuneration for the referral of patients whose care will be paid by federal governmental programs or fee-splitting arrangements between health care providers that are designed to induce the referral of patients to a provider for medical products and services. Furthermore, many states prohibit business corporations from providing or holding themselves out as a provider of medical care.
In addition, the Stark Law broadly defines the scope of prohibited physician referrals under federal health care programs to providers with which they have ownership or other financial arrangements. Many states have adopted, or are considering, legislative proposals similar to these laws, some of which extend beyond federal health care programs, to prohibit the payment or receipt of remuneration for the referral of patients and physician referrals regardless of the source of the payment for the care.
We also are subject to potential lawsuits under a federal whistle-blower statute designed to combat fraud and abuse in the health care industry, known as the federal False Claims Act. These lawsuits can involve significant monetary awards to private plaintiffs who successfully bring these suits. When a private party brings a qui tam action under the False Claims Act, it files the complaint with the court under seal, and the defendant will generally not be aware of the lawsuit until the government makes a determination whether it will intervene and take a lead in the litigation. Even if, during an investigation, the court partially unseals a complaint to allow the government and a defendant to work toward a resolution of the complaint's allegations, the defendant is prohibited from revealing to anyone the existence of the complaint or that the partial unsealing has occurred.
These laws and regulations are complex and limited judicial or regulatory interpretation exists. We cannot assure you that governmental officials charged with responsibility for enforcing the provisions of these laws and regulations will not assert that one or more of our arrangements are in violation of the provisions of such laws and regulations.
The regulatory environment surrounding the post–acute and long–term care industry has intensified, particularly for larger for–profit, multi–facility providers like us. The federal government has imposed extensive enforcement policies resulting in a significant increase in the number of inspections, citations of regulatory deficiencies and other regulatory sanctions, including terminations from the Medicare and Medicaid programs, denials of payment for new Medicare and Medicaid admissions and civil monetary penalties.
If we fail to obtain or renew required regulatory approvals or licenses or fail to comply, or are perceived as failing to comply, with other extensive laws and regulations applicable to our business, we could have our licenses suspended or revoked, become ineligible to receive government program reimbursement, be required to refund amounts received from Medicare, Medicaid or private payors, suffer civil or criminal penalties, suffer damage to our reputation in various markets or be required to make significant changes to our operations. Any of these sanctions could have a material adverse effect on our operations and financial condition. Furthermore, should we lose licenses or certifications for many of our facilities as a result of regulatory action or otherwise, we could be deemed in default under some of our agreements, including agreements governing outstanding indebtedness.
We have established policies and procedures that we believe are sufficient to ensure that we will operate in substantial compliance with these anti–fraud and abuse requirements. From time to time, we may seek guidance as to the interpretation of these laws; however, there can be no assurance that such laws will ultimately be interpreted in a manner consistent with our practices. In addition, we could be forced to expend considerable resources responding to an investigation or other enforcement action under these laws or regulations. While we believe that our business practices are consistent with Medicare and Medicaid criteria, those criteria are often vague and subject to change and interpretation. We are unable to predict the future course of federal, state and local regulation or legislation, including Medicare and Medicaid statutes and regulations, or the intensity of federal and state enforcement actions. Aggressive anti–fraud actions have had and could have an adverse effect on our financial position, results of operations and cash flows. See Item 1, "Business – Government Regulation".
We are unable to predict the ultimate impact of COVID-19 pandemic stimulus or relief legislation or the effect that such legislation or other government responses intended to assist healthcare providers in responding to the COVID-19 pandemic may have on our business, financial condition, results of operations, or cash flows. In response to the COVID-19 pandemic, federal and state governments have passed legislation, promulgated regulations and taken other administrative actions intended to assist healthcare providers in providing care to COVID-19 and other patients and to provide financial relief to healthcare providers. Together, the CARES Act, the Paycheck Protection Program and Health Care Enhancement Act (“PPPHCE Act”), the Consolidated Appropriations Act, 2021 (“CAA”) and the American Rescue Plan Act of 2021 authorized over $186 billion in funding to be distributed to health care providers through the Provider Relief Fund. These funds were intended to reimburse eligible providers, including public entities and Medicare and/or Medicaid-enrolled providers and suppliers, for healthcare-related expenses or lost revenues attributable to COVID-19. Recipients were not required to repay these funds, provided that they attest to and comply with certain terms and conditions, including not using Provider Relief Fund payments to reimburse expenses or losses that other sources are obligated to reimburse and submitting reports as required by HHS. Recipients of Provider Relief Fund payments are subject to audit requirements, and we expect that recipients of funds from the Provider Relief Fund will be subject to significant scrutiny by the federal government. We have structured our use of these funds in accordance with the terms and conditions, but federal regulators may disagree with our interpretation of these terms and conditions and require that we repay some or all amounts received at our facilities or impose other penalties.
Beyond financial assistance, federal and state governments have enacted legislation and established regulations intended to expand access to and payment for telehealth services, increase access to medical supplies and equipment, prioritize review of drug applications to help with shortages of emergency drugs, and ease various legal and regulatory burdens on health care providers. HHS and CMS have announced other flexibilities for health care providers in response to COVID-19, such as relief from data submission requirements and measure suppression policies for providers participating in certain quality reporting programs. It is unclear how changes to these and other value-based programs will affect our financial condition.
There is still a high degree of uncertainty surrounding the implementation of the CARES Act and related legislation passed in response to the COVID-19 pandemic, and the pandemic continues to evolve. Some of the measures allowing for flexibility in delivery of care and various financial supports for health care providers are available only for the duration of the national public health emergency (“PHE”) declared by HHS as a result of the pandemic. The Biden administration announced on January 30, 2023 that the COVID-19 public health emergency is set to end on May 11, 2023. The federal government may consider additional stimulus and relief efforts, but we are unable to predict whether additional measures will be enacted or their impact. There can be no assurance as to the total amount of financial and other types of assistance we will ultimately receive under stimulus and relief legislation, and it is difficult to predict the impact of such legislation on our operations. Further, there can be no assurance that the terms and conditions of the Provider Relief Fund or other programs will not change in ways that affect funding we may receive, our ability to comply with such terms and conditions in the future or our eligibility to participate. We continue to assess the potential impact of COVID-19 and government responses to the pandemic, including the enactment and implementation of the CARES Act and related legislation on our business, financial condition, results of operations and cash flows.
Our business may be impacted by healthcare reform efforts. In recent years, the U.S. Congress and certain state legislatures have considered and passed a large number of laws intended to result in significant changes to the healthcare industry, including the ACA. The ACA affects how healthcare services are delivered and reimbursed through the expansion of public and private health insurance coverage, reduction of growth in Medicare and Medicaid spending, and the establishment and expansion of programs that tie reimbursement to quality and integration. The ACA has been subject to legislative and regulatory changes and court challenges. Although the current presidential administration has indicated that it generally intends to protect and strengthen the ACA, it is possible that there may be continued changes to the ACA, its implementation or its interpretation. Changes by Congress or government agencies could eliminate or alter provisions beneficial to us, while leaving in place provisions reducing our reimbursement or otherwise negatively impacting our business.
There is also uncertainty regarding whether, when and what other health reform measures will be adopted, and the impact of such efforts on providers as well as other healthcare industry participants. Some members of Congress have proposed expanding government-funded coverage, including proposals to expand coverage of federally-funded insurance programs as an alternative to private insurance or to establish a single payor system (such reforms are often referred to as “Medicare for All”), and some states have implemented or proposed public health insurance options.
In addition, CMS administrators may make changes to Medicaid payment models or grant additional flexibilities to states in the administration of state Medicaid programs, including by expanding the scope of waivers under which states may implement Medicaid expansion provisions, impose different eligibility or enrollment restrictions, or otherwise implement programs that vary from federal standards. Other industry participants, such as private payors, may also introduce financial or delivery system reforms. We are unable to predict the nature and success of such initiatives. Healthcare reform initiatives may have an adverse effect on our business, financial condition, and operating results.
We are required to comply with laws governing the transmission and privacy and security of health information. The Health Insurance Portability and Accountability Act of 1996, or ("HIPAA"), requires the use of uniform electronic data transmission standards for healthcare claims and payment transactions submitted or received electronically. In addition, as required by HIPAA, the HHS has issued privacy and security regulations that extensively regulate the use and disclosure of individually identifiable health information (known as Protected Health Information, or PHI) and require covered entities, including healthcare providers and health plans, and vendors known as "business associates," to implement administrative, physical and technical safeguards to protect the security of PHI. Covered entities must report breaches of unsecured PHI without unreasonable delay to affected individuals, HHS and, in the case of larger breaches, the media. The privacy, security and breath notification regulations have imposed, and will continue to impose, significant compliance costs on our operations.
There are numerous other laws and legislative and regulatory initiatives at the federal and state levels addressing privacy and security concerns. These laws vary and may impose additional obligations or penalties. For example, additional federal and state obligations may apply to behavioral, addictive disorder and other types of sensitive information. Further, various state laws and regulations may require us to notify affected individuals in the event of a data breach involving individually identifiable information (even if no health-related information is involved). In addition, the Federal Trade Commission uses its consumer protection authority to initiate enforcement actions in response to data breaches. To the extent we fail to comply with one or more federal and/or state privacy and security requirements or if we are found to be responsible for the non-compliance of our vendors, we could be subject to substantial fines or penalties, as well as third-party claims, and suffer harm to our reputation, which could have a material adverse effect on our business, financial position, results of operations and liquidity.
In addition, health care providers and industry participants are also subject to a growing number of requirements intended to promote the interoperability and exchange of patient health information. For example, most health care providers and certain other entities are subject to information blocking restrictions pursuant to the 21st Century Cures Act that prohibit practices that are likely to interfere with the access, exchange or use of electronic health information, except as required by law or specified by HHS as a reasonable and necessary activity.
We are subject to employment-related laws and regulations which could increase our cost of doing business and subject us to significant back pay awards, fines and lawsuits. Our operations are subject to a variety of federal, state and local employment-related laws and regulations, including, but not limited to, the U.S. Fair Labor Standards Act, which governs such matters as minimum wages, the Family Medical Leave Act, overtime pay, compensable time, record keeping and other working conditions, Title VII of the Civil Rights Act, the Employee Retirement Income Security Act, the Americans with Disabilities Act, the National Labor Relations Act, regulations of the Equal Employment Opportunity Commission, regulations of the Office of Civil Rights, regulations of the Department of Labor (DOL), federal and state wage and hour laws, and a variety of similar laws enacted by the federal and state governments that govern these and other employment-related matters. Because labor represents such a large portion of our operating costs, compliance with these evolving federal and state laws and regulations could substantially increase our cost of doing business while failure to do so could subject us to significant back pay awards, fines and lawsuits. In addition, federal proposals to introduce a system of mandated health insurance and flexible work time and other similar initiatives could, if implemented, adversely affect our operations. Our failure to comply with federal and state employment-related laws and regulations could have a material adverse effect on our business, financial position, results of operations and liquidity.
Our business is subject to a variety of federal, state and local environmental laws and regulations. As a healthcare provider, we face regulatory requirements in areas of air and water quality control, medical and low–level radioactive waste management and disposal, asbestos management, response to mold and lead–based paint in our facilities and employee safety.
As an operator of healthcare facilities, we also may be required to investigate and remediate hazardous substances that are located on and/or under the property, including any such substances that may have migrated off, or may have been discharged or transported from the property. Part of our operations involves the handling, use, storage, transportation, disposal and discharge of medical, biological, infectious, toxic, flammable, and other hazardous materials, wastes, pollutants, or contaminants. In addition, we are sometimes unable to determine with certainty whether prior uses of our facilities and properties or surrounding properties may have produced continuing environmental contamination or noncompliance, particularly where the timing or cost of making such determinations is not deemed cost effective. These activities, as well as the possible presence of such materials in, on and under our properties, may result in damage to individuals, property, or the environment; may interrupt operations or increase costs; may result in legal liability, damages, injunctions or fines; may result in investigations, administrative proceedings, penalties or other governmental agency actions; and may not be covered by insurance.
We believe that we are in material compliance with applicable environmental and occupational health and safety requirements. However, we cannot assure you that we will not encounter environmental liabilities in the future, and such liabilities may result in material adverse consequences to our operations or financial condition.
We are subject to federal and state income taxes. Changes in tax laws and regulations or the interpretation of such laws could adversely affect our position on income taxes and estimated income liabilities. Uncertain tax positions may arise where tax laws may allow for alternative interpretations or where the timing of recognition of income is subject to judgment. We believe we have adequate provisions for unrecognized tax benefits related to uncertain tax positions. Although we believe we have accurately estimated our tax liabilities, uncertainty of interpretation by various tax authorities and the possibility that there are issues that have not been recognized by management could result in additional tax liability. We believe that our liabilities reflect the anticipated outcome of known uncertain tax positions in conformity with ASC Topic 740 Income Taxes.
We are also subject to regular reviews, examinations, and audits by the Internal Revenue Service and other taxing authorities with respect to our taxes. There are uncertainties and ambiguities in the application of the Tax Cuts and Jobs Act of 2017 ("Tax Act") and it is possible that the IRS could issue subsequent guidance or take positions on audit that differ from our interpretations and assumptions. Although we believe our tax estimates are reasonable, if a taxing authority disagrees with the positions we have taken, we could face additional tax liability, including interest and penalties. Our effective tax rate could be adversely affected by changes in the mix of earnings in states with different statutory tax rates, changes in the valuation of deferred tax assets and liabilities, change in tax laws and regulations, changes in our interpretations of tax laws, including the Tax Act. Unanticipated changes in our tax rates or exposure to additional income tax liabilities could affect our profitability. There can be no assurance that payment of such additional amounts upon final adjudication of any disputes will not have a material impact on our results of operations and financial position.
Risks Related to Our Structure and Public Company Compliance
Failure to maintain effective internal controls in accordance with Section 404 of the Sarbanes–Oxley Act could result in a restatement of our financial statements, cause investors to lose confidence in our financial statements and our company and have a material adverse effect on our business and stock price. We produce our consolidated financial statements in accordance with the requirements of U.S. GAAP. Effective internal controls are necessary for us to provide reliable financial reports to help mitigate the risk of fraud and to operate successfully as a publicly traded company. As a public company, we are required to document and test our internal control procedures in order to satisfy the requirements of Section 404 of the Sarbanes–Oxley Act of 2002, or Section 404, which requires annual management assessments of the effectiveness of our internal controls over financial reporting.
Testing and maintaining internal controls can divert our management's attention from other matters that are important to our business. We may not be able to conclude on an ongoing basis that we have effective internal controls over financial reporting in accordance with Section 404 or our independent registered public accounting firm may not be able to issue an unqualified report if we conclude that our internal controls over financial reporting are not effective. If either we are unable to conclude that we have effective internal controls over financial reporting or our independent registered public accounting firm is unable to provide us with an unqualified report as required by Section 404, investors could lose confidence in our reported financial information and our company, which could result in a decline in the market price of our common stock, and cause us to fail to meet our reporting obligations in the future, which in turn could impact our ability to raise additional financing if needed in the future.
Increasing costs of being publicly owned are likely to impact our future consolidated financial position and results of operations. In connection with the Sarbanes–Oxley Act of 2002, we are subject to rules requiring our management to report on the effectiveness of our internal control over financial reporting. If we fail to have effective internal controls and procedures for financial reporting in place, we could be unable to provide timely and reliable financial information which could, in turn, have an adverse effect on our business, results of operations, financial condition and cash flows.
Significant regulatory changes, including the Sarbanes–Oxley Act and rules and regulations promulgated as a result of the Sarbanes–Oxley Act, have increased, and in the future, are likely to further increase general and administrative costs. In order to comply with the Sarbanes–Oxley Act of 2002, the listing standards of the NYSE exchange, and rules implemented by the SEC, we have had to hire additional personnel and utilize additional outside legal, accounting and advisory services, and may continue to require such additional resources. Moreover, in the rapidly changing regulatory environment in which we operate, there is significant uncertainty as to what will be required to comply with many of the regulations. As a result, we may be required to spend substantially more than we currently estimate, and may need to divert resources from other activities, as we develop our compliance plans.
Provision for losses in our financial statements may not be adequate. Loss provisions in our financial statements for self–insured programs are made on an undiscounted basis in the relevant period. These provisions are based on internal and external evaluations of the merits of individual claims, analysis of claims history and independent actuarially determined estimates. Our management reviews the methods of determining these estimates and establishing the resulting accrued liabilities frequently, with any material adjustments resulting from being reflected in current earnings. Although we believe that our provisions for self–insured losses in our financial statements are adequate, the ultimate liability may be in excess of the amounts recorded. In the event the provisions for losses reflected in our financial statements are inadequate, our financial condition and results of operations may be materially affected.
Implementation of new information technology could cause business interruptions and negatively affect our profitability and cash flows. We continue to refine and implement our information technology to improve customer service, enhance operating efficiencies and provide more effective management of business operations. Implementation of information technology carries risks such as cost overruns, project delays and business interruptions and delays. If we experience a material business interruption as a result of the implementation of our existing or future information technology infrastructure or are unable to obtain the projected benefits of this new infrastructure, it could adversely affect us and could have a material adverse effect on our business, results of operations, financial condition and cash flows.
We depend on the proper function and availability of our information systems. We are dependent on the proper function and availability of our information systems. Though we have taken steps to protect the safety and security of our information systems and the data maintained within those systems, there can be no assurance that our safety and security measures and disaster recovery plan will prevent damage or interruption of our systems and operations, and we may be vulnerable to losses associated with the improper functioning, security breach or unavailability of our information systems. Failure to maintain proper function and availability of our information systems could have a material adverse effect on our business, financial position, results of operations and liquidity.
In addition, certain software supporting our business and information systems are licensed to us by independent software developers. Our inability or the inability of these developers, to continue to maintain and upgrade our information systems and software could disrupt or reduce the efficiency of our operations. In addition, costs and potential problems and interruptions associated with the implementation of new or upgraded systems and technology or with maintenance or adequate support of existing systems also could disrupt or reduce the efficiency of our operations and could have a material adverse effect on our business, financial position, results of operations and liquidity.
Cybersecurity risks could harm our ability to operate effectively. Cybersecurity refers to the combination of technologies, processes and procedures established to protect information technology systems and data from unauthorized access, attack, or damage. We rely on our information systems to provide security for processing, transmission and storage of confidential patient, resident, employee, other consumer information, such as personally identifiable information, including information relating to health protected by HIPAA. Although we have taken steps to protect the security of our information systems, medical devices that store sensitive data, and the data maintained in those systems and devices, it is possible that our safety and security measures will not prevent improper functioning or the improper access or disclosure of personally identifiable information such as in the event of cyber-attacks. We may be at increased risk because we outsource certain services or functions to, or have systems that interface with, third parties. Some of these third parties may store or have access to our data and may not have effective controls, processes, or practices to protect our information from attack, damage, or unauthorized access. A breach or attack, including those caused by updates and other releases, affecting any of these third parties could harm our business. In addition, the COVID-19 pandemic may have an adverse impact on our information technology systems and our ability to securely preserve confidential information, including risks associated with telecommuting issues when our employees work remotely.
If personally identifiable information of our patients or others is improperly accessed, tampered with or distributed, we may incur significant costs to remediate possible injury to the affected patients, and we may be subject to sanctions and civil or criminal penalties if we are found to be in violation of the privacy or security rules under HIPAA or other similar federal or state laws protecting confidential personally identifiable information.
Security breaches, including physical or electronic break–ins, computer viruses, attacks by hackers and similar breaches can create system disruptions or shutdowns or the unauthorized disclosure of confidential information. Additionally, healthcare businesses are increasingly targets of cyberattacks, whereby hackers disrupt business operations or obtain protected health information, often demanding large ransoms. As cyber threats continue to evolve, we may be required to expend significant additional resources to continue to modify or enhance our protective measures or to investigate and remediate any cybersecurity vulnerabilities. The occurrence of any of these events could result in harm to patients; business interruptions or delays; the loss, misappropriation, corruption, or unauthorized access of data; litigation and potential liability under privacy, security and consumer protection laws or other applicable laws; reputational damage; or federal and state governmental inquiries. Any failure to maintain proper functionality and security of our information systems could have a material adverse effect on our business, financial condition, and results of operations.
We may not be able to meet all our capital needs. We cannot assure you that our business will generate cash flow from operations that anticipated revenue growth and improvement of operating efficiencies will be realized or that future borrowings will be available to us in an amount sufficient to enable us to service any future indebtedness or to fund our other liquidity needs. We may need to incur indebtedness, sell assets, or make certain discretionary capital expenditures.
The performances of our fixed–income and our equity investment portfolios are subject to a variety of investment risks. Our investment portfolios are comprised principally of fixed–income securities and common equities. Our fixed–income portfolio is actively managed by an investment group and includes short–term investments and fixed–maturity securities. The performances of our fixed–income and our equity portfolios are subject to a number of risks, including:
| |
● |
Interest rate risk – the risk of adverse changes in the value of fixed–income securities as a result of increases in market interest rates. |
| |
● |
Investment credit risk – the risk that the value of certain investments may decrease in value due to the deterioration in financial condition of, or the liquidity available to, one or more issuers of those securities or, in the case of asset–backed securities, due to the deterioration of the loans or other assets that underlie the securities, which, in each case, also includes the risk of permanent loss. |
| |
● |
Concentration risk – the risk that the portfolio may be too heavily concentrated in the securities of National Health Investors “NHI,” or certain sectors or industries, which could result in a significant decrease in the value of the portfolio in the event of a deterioration of the financial condition, performance, or outlook of NHI, or those certain sectors or industries. |
| |
● |
Liquidity risk – the risk that we will not be able to convert investments into cash on favorable terms and on a timely basis or that we will not be able to sell them at all, when we desire to do so. Disruptions in the financial markets or a lack of buyers for the specific securities that we are trying to sell, could prevent us from liquidating securities or cause a reduction in prices to levels that are not acceptable to us. |
In addition, the success of our investment strategies and asset allocations in the fixed–income portfolio may vary depending on the market environment. The fixed–income portfolio's performance also may be adversely impacted if, among other factors: there is a lack of transparency regarding the underlying businesses of the issuers of the securities that we purchase; credit ratings assigned to such securities by nationally recognized credit rating agencies are based on incomplete information or prove unwarranted; or our risk mitigation strategies are ineffective for the applicable market conditions.
The common equity portfolio is subject to general movements in the values of equity markets and to the changes in the prices of the securities we hold. Equity markets, sectors, industries, and individual securities may be subject to high volatility and to long periods of depressed or declining valuations.
If the fixed–income or equity portfolios, or both, were to suffer a decrease in value due to market, sector, or issuer–specific conditions to a substantial degree, our liquidity, financial position, and financial results could be materially adversely affected.
Our stock price is volatile and fluctuations in our operating results, quarterly earnings and other factors may result in declines in the price of our common stock. Equity markets are prone to, and in the last few years have experienced, extreme price and volume fluctuations. Volatility over the past few years has had a significant impact on the market price of securities issued by many companies, including us and other companies in the healthcare industry. If we are unable to operate our businesses as profitably as we have in the past or as our stockholders expect us to in the future, the market price of our common stock will likely decline as stockholders could sell shares of our common stock when it becomes apparent that the market expectations may not be realized. In addition to our operating results, many economic and other factors beyond our control could have an adverse effect on the price of our common stock including:
| |
● |
general economic conditions; |
| |
● |
developments generally affecting the healthcare industry; |
| |
● |
strategic actions, such as acquisitions or restructurings, or the introduction of new services by us or our competitors; |
| |
● |
new laws or regulations or new interpretations of existing laws or regulations applicable to our business; |
| |
● |
litigation and governmental investigations; |
| |
● |
changes in accounting standards, policies, guidance, interpretations or principles; |
| |
● |
investor perceptions of us and our business; |
| |
● |
actions by institutional or other large stockholders; |
| |
● |
quarterly variations in operating results; |
| |
● |
changes in financial estimates and recommendations by securities analysts; |
| |
● |
press releases or negative publicity relating to our competitors or us or relating to trends in health care; |
| |
● |
sales of stock by insiders; |
| |
● |
natural disasters, terrorist attacks and pandemics; and |
| |
● |
additions or departures of key personnel. |
We may not be able to pay or maintain dividends and the failure to do so would adversely affect our stock price. We currently pay a quarterly dividend on our common stock and our Board intends to continue to pay a quarterly dividend. However, our ability to pay and maintain cash dividends is based on many factors, including our financial condition, funds from operations, the level of our capital expenditures and future business prospects, our ability to make and finance acquisitions, anticipated operating cost levels, the level of demand for our beds, the rates we charge and actual results that may vary substantially from estimates. Some of the factors are beyond our control and a change in any such factor could affect our ability to pay or maintain dividends. The failure to pay or maintain dividends could adversely affect our stock price.
| ITEM 1B. |
UNRESOLVED STAFF COMMENTS |
None.
| Skilled Nursing Facilities |
|
|
|
|
|
| State |
|
City |
|
Center Name |
|
Affiliation |
|
Licensed Beds |
| Alabama |
|
Anniston |
|
NHC HealthCare, Anniston |
|
Leased(1) |
|
151 |
| |
|
Moulton |
|
NHC HealthCare, Moulton |
|
Leased(1) |
|
136 |
| |
|
|
|
|
|
|
|
|
| Georgia |
|
Fort Oglethorpe |
|
NHC HealthCare, Fort Oglethorpe |
|
Owned |
|
135 |
| |
|
Rossville |
|
NHC HealthCare, Rossville |
|
Owned |
|
112 |
| |
|
|
|
|
|
|
|
|
| Kentucky |
|
Glasgow |
|
NHC HealthCare, Glasgow |
|
Leased(1) |
|
194 |
| |
|
|
|
|
|
|
|
|
| Missouri |
|
Desloge |
|
NHC HealthCare, Desloge |
|
Leased(1) |
|
120 |
| |
|
Independence |
|
The Villages of Jackson Creek |
|
Leased |
|
120 |
| |
|
Independence |
|
The Villages of Jackson Creek Memory Care |
|
Leased |
|
70 |
| |
|
Joplin |
|
NHC HealthCare, Joplin |
|
Leased(1) |
|
126 |
| |
|
Kennett |
|
NHC HealthCare, Kennett |
|
Leased(1) |
|
170 |
| |
|
Macon |
|
Macon Health Care Center |
|
Owned |
|
120 |
| |
|
Osage Beach |
|
Osage Beach Rehabilitation and Health Care Center |
|
Owned |
|
94 |
| |
|
St. Charles |
|
NHC HealthCare, St. Charles |
|
Leased(1) |
|
120 |
| |
|
St. Louis |
|
NHC HealthCare, Maryland Heights |
|
Leased(1) |
|
220 |
| |
|
St. Peters |
|
Villages of St. Peters |
|
Leased |
|
130 |
| |
|
Springfield |
|
Springfield Rehabilitation and Health Care Center |
|
Leased |
|
146 |
| |
|
West Plains |
|
NHC HealthCare, West Plains |
|
Owned |
|
114 |
| |
|
|
|
|
|
|
|
|
| South Carolina |
|
Anderson |
|
NHC HealthCare, Anderson |
|
Leased(1) |
|
290 |
| |
|
Bluffton |
|
NHC HealthCare, Bluffton |
|
Owned |
|
120 |
| |
|
Charleston |
|
NHC HealthCare, Charleston |
|
Owned |
|
132 |
| |
|
Clinton |
|
NHC HealthCare, Clinton |
|
Owned |
|
131 |
| |
|
Columbia |
|
NHC HealthCare, Parklane |
|
Owned |
|
180 |
| |
|
Greenwood |
|
NHC HealthCare, Greenwood |
|
Leased(1) |
|
152 |
| |
|
Greenville |
|
NHC HealthCare, Greenville |
|
Owned |
|
176 |
| |
|
Laurens |
|
NHC HealthCare, Laurens |
|
Leased(1) |
|
176 |
| |
|
Lexington |
|
NHC HealthCare, Lexington |
|
Owned |
|
170 |
| |
|
Mauldin |
|
NHC HealthCare, Mauldin |
|
Owned |
|
180 |
| |
|
Murrells Inlet |
|
NHC HealthCare, Garden City |
|
Owned |
|
148 |
| |
|
North Augusta |
|
NHC HealthCare, North Augusta |
|
Owned |
|
192 |
| |
|
Sumter |
|
NHC HealthCare, Sumter |
|
Managed |
|
138 |
| |
|
|
|
|
|
|
|
|
| Tennessee |
|
Athens |
|
NHC HealthCare, Athens |
|
Leased(1) |
|
86 |
| |
|
Chattanooga |
|
NHC HealthCare, Chattanooga |
|
Leased(1) |
|
200 |
| |
|
Columbia |
|
NHC HealthCare, Columbia |
|
Owned |
|
106 |
| |
|
Columbia |
|
NHC-Maury Regional Transitional Care Center |
|
Owned |
|
112 |
| |
|
Cookeville |
|
NHC HealthCare, Cookeville |
|
Managed |
|
104 |
| |
|
Dickson |
|
NHC HealthCare, Dickson |
|
Leased(1) |
|
191 |
| |
|
Dunlap |
|
NHC HealthCare, Sequatchie |
|
Leased(1) |
|
110 |
| |
|
Farragut |
|
NHC HealthCare, Farragut |
|
Owned |
|
106 |
| |
|
Franklin |
|
NHC Place, Cool Springs |
|
Owned |
|
180 |
| |
|
Franklin |
|
NHC HealthCare, Franklin |
|
Leased(1) |
|
80 |
| |
|
Gallatin |
|
NHC Place, Sumner |
|
Owned |
|
92 |
| |
|
Hendersonville |
|
NHC HealthCare, Hendersonville |
|
Leased(1) |
|
122 |
| |
|
Johnson City |
|
NHC HealthCare, Johnson City |
|
Leased(1) |
|
167 |
| |
|
Kingsport |
|
NHC HealthCare, Kingsport |
|
Owned |
|
90 |
| |
|
Knoxville |
|
NHC HealthCare, Fort Sanders |
|
Owned |
|
166 |
| |
|
Knoxville |
|
Holston Health & Rehabilitation Center |
|
Owned |
|
94 |
| |
|
Knoxville |
|
NHC HealthCare, Knoxville |
|
Owned |
|
127 |
| |
|
Lawrenceburg |
|
NHC HealthCare, Lawrenceburg |
|
Managed |
|
96 |
| |
|
Lawrenceburg |
|
NHC HealthCare, Scott |
|
Leased(1) |
|
60 |
| |
|
Lewisburg |
|
NHC HealthCare, Lewisburg |
|
Leased(1) |
|
100 |
| |
|
Lewisburg |
|
NHC HealthCare, Oakwood |
|
Leased(1) |
|
60 |
| |
|
McMinnville |
|
NHC HealthCare, McMinnville |
|
Leased(1) |
|
115 |
| |
|
Milan |
|
NHC HealthCare, Milan |
|
Leased(1) |
|
117 |
| |
|
Murfreesboro |
|
AdamsPlace |
|
Owned |
|
90 |
| |
|
Murfreesboro |
|
NHC HealthCare, Murfreesboro |
|
Managed |
|
181 |
| |
|
Nashville |
|
Lakeshore, Heartland |
|
Managed |
|
66 |
| |
|
Nashville |
|
Lakeshore, The Meadows |
|
Managed |
|
113 |
| |
|
Nashville |
|
The Health Center of Richland Place |
|
Managed |
|
107 |
| |
|
Nashville |
|
NHC Place at The Trace |
|
Owned |
|
90 |
| |
|
Nashville |
|
West Meade Place |
|
Managed |
|
120 |
| |
|
Oak Ridge |
|
NHC HealthCare, Oak Ridge |
|
Managed |
|
120 |
| |
|
Pulaski |
|
NHC HealthCare, Pulaski |
|
Leased(1) |
|
102 |
| |
|
Smithville |
|
NHC HealthCare, Smithville |
|
Leased(1) |
|
114 |
| |
|
Somerville |
|
NHC HealthCare, Somerville |
|
Leased(1) |
|
72 |
| |
|
Sparta |
|
NHC HealthCare, Sparta |
|
Leased(1) |
|
90 |
| |
|
Springfield |
|
NHC HealthCare, Springfield |
|
Owned |
|
107 |
| |
|
Tullahoma |
|
NHC HealthCare, Tullahoma |
|
Owned |
|
90 |
| |
|
|
|
|
|
|
|
|
| Virginia |
|
Bristol |
|
NHC HealthCare, Bristol |
|
Leased(1) |
|
120 |
| Behavioral Health Hospitals |
|
|
|
|
| State |
|
City |
|
Center Name |
|
Affiliation |
|
Licensed Beds |
| Missouri |
|
Maryland Heights |
|
Maryland Heights Center for Behavioral Health |
|
Owned |
|
16 |
| |
|
Osage Beach |
|
Osage Beach Center for Cognitive Disorders |
|
Owned |
|
16 |
| |
|
|
|
|
|
|
|
|
| Tennessee |
|
Knoxville |
|
Knoxville Center for Behavioral Medicine |
|
Owned(2) |
|
64 |
| Assisted Living Units |
|
|
|
|
| |
|
|
|
|
|
|
|
|
| State |
|
City |
|
Center Name |
|
Affiliation |
|
Units |
| Alabama |
|
Anniston |
|
NHC Place/Anniston |
|
Owned |
|
67 |
| |
|
|
|
|
|
|
|
|
| Kentucky |
|
Glasgow |
|
NHC HealthCare, Glasgow |
|
Leased(1) |
|
12 |
| |
|
|
|
|
|
|
|
|
| Missouri |
|
St. Charles |
|
Lake St. Charles Retirement Center |
|
Leased(1) |
|
26 |
| |
|
Independence |
|
The Villages of Jackson Creek |
|
Leased |
|
52 |
| |
|
St. Peters |
|
Villages of St. Peters |
|
Leased |
|
52 |
| |
|
St. Peters |
|
Villages of St. Peters Memory Care |
|
Owned |
|
60 |
| |
|
|
|
|
|
|
|
|
| South Carolina |
|
Bluffton |
|
The Palmettos of Bluffton |
|
Owned |
|
78 |
| |
|
Charleston |
|
The Palmettos of Charleston |
|
Owned |
|
60 |
| |
|
Columbia |
|
The Palmettos of Parklane |
|
Owned |
|
75 |
| |
|
Greenville |
|
The Palmettos of Mauldin |
|
Owned |
|
45 |
| |
|
Murrells Inlet |
|
The Palmettos of Garden City |
|
Owned |
|
80 |
| |
|
|
|
|
|
|
|
|
| Tennessee |
|
Dickson |
|
NHC HealthCare, Dickson |
|
Leased(1) |
|
20 |
| |
|
Farragut |
|
NHC Place, Farragut |
|
Owned |
|
84 |
| |
|
Farragut |
|
NHC Place, Cavette Hill |
|
Owned |
|
60 |
| |
|
Franklin |
|
NHC Place, Cool Springs |
|
Owned |
|
89 |
| |
|
Gallatin |
|
NHC Place, Sumner |
|
Owned |
|
80 |
| |
|
Murfreesboro |
|
AdamsPlace |
|
Owned |
|
106 |
| |
|
Nashville |
|
Lakeshore Heartland |
|
Managed |
|
9 |
| |
|
Nashville |
|
Lakeshore, The Meadows |
|
Managed |
|
10 |
| |
|
Nashville |
|
Richland Place |
|
Managed |
|
24 |
| |
|
Nashville |
|
The Place at the Trace |
|
Owned |
|
80 |
| |
|
Smithville |
|
NHC HealthCare, Smithville |
|
Leased(1) |
|
6 |
| |
|
Somerville |
|
NHC HealthCare, Somerville |
|
Leased(1) |
|
6 |
| Retirement Apartments |
|
|
|
| |
|
|
|
|
|
|
|
|
| State |
|
City |
|
Retirement Apartments |
|
Affiliation |
|
Units |
| Missouri |
|
St. Charles |
|
Lake St. Charles Retirement Apts. |
|
Leased(1) |
|
152 |
| |
|
|
|
|
|
|
|
|
| Tennessee |
|
Chattanooga |
|
Parkwood Retirement Apartments |
|
Leased(1) |
|
30 |
| |
|
Johnson City |
|
Colonial Hill Retirement Apartments |
|
Leased(1) |
|
63 |
| |
|
Murfreesboro |
|
AdamsPlace |
|
Owned |
|
93 |
| |
|
Nashville |
|
Richland Place Retirement Apts. |
|
Managed |
|
137 |
| Homecare Agencies |
| |
|
|
|
|
| State |
|
City |
|
Homecare Agencies |
| Florida |
|
Chipley |
|
NHC HomeCare of Chipley |
| |
|
Crawfordville |
|
NHC HomeCare of Crawfordville |
| |
|
Merritt Island |
|
NHC HomeCare of Merritt Island |
| |
|
Panama City |
|
NHC HomeCare of Panama City |
| |
|
Port St. Joe |
|
NHC HomeCare of Port St. Joe |
| |
|
Quincy |
|
NHC HomeCare of Quincy |
| |
|
Vero Beach |
|
NHC HomeCare of Vero Beach |
| |
|
|
|
|
| South Carolina |
|
Aiken |
|
NHC HomeCare of Aiken |
| |
|
Anderson |
|
NHC HomeCare of Anderson |
| |
|
Bluffton |
|
NHC HomeCare of Beaufort |
| |
|
Greenville |
|
NHC HomeCare of Greenville |
| |
|
Greenwood |
|
NHC HomeCare of Greenwood |
| |
|
Laurens |
|
NHC HomeCare of Laurens |
| |
|
Murrells Inlet |
|
NHC HomeCare of Murrells Inlet |
| |
|
Summerville |
|
NHC HomeCare of Low Country |
| |
|
West Columbia |
|
NHC HomeCare of Midlands |
| |
|
|
|
|
| Tennessee |
|
Athens |
|
NHC HomeCare of Athens |
| |
|
Chattanooga |
|
NHC HomeCare of Chattanooga |
| |
|
Columbia |
|
NHC HomeCare of Columbia |
| |
|
Cookeville |
|
NHC HomeCare of Cookeville |
| |
|
Dickson |
|
NHC HomeCare of Dickson |
| |
|
Franklin |
|
NHC HomeCare of Franklin |
| |
|
Hendersonville |
|
NHC HomeCare of Hendersonville |
| |
|
Johnson City |
|
NHC HomeCare of Johnson City |
| |
|
Knoxville |
|
NHC HomeCare of Knoxville |
| |
|
Lawrenceburg |
|
NHC HomeCare of Lawrenceburg |
| |
|
Lewisburg |
|
NHC HomeCare of Lewisburg |
| |
|
McMinnville |
|
NHC HomeCare of McMinnville |
| |
|
Milan |
|
NHC HomeCare of Milan |
| |
|
Murfreesboro |
|
NHC HomeCare of Murfreesboro |
| |
|
Nashville |
|
Ascension at Home St. Thomas(3) |
| |
|
Pulaski |
|
NHC HomeCare of Pulaski |
| |
|
Somerville |
|
NHC HomeCare of Somerville |
| |
|
Sparta |
|
NHC HomeCare of Sparta |
| |
|
Springfield |
|
NHC HomeCare of Springfield |
| Hospice Agencies |
|
| |
|
|
|
|
|
| State |
|
City |
|
Hospice Agencies |
|
| Georgia |
|
Rossville |
|
Caris Healthcare – Rossville |
|
| |
|
|
|
|
|
| Missouri |
|
St. Louis |
|
Caris Healthcare – St. Louis |
|
| |
|
|
|
|
|
| South Carolina |
|
Anderson |
|
Caris Healthcare – Anderson |
|
| |
|
Bluffton |
|
Caris Healthcare – Bluffton |
|
| |
|
Charleston |
|
Caris Healthcare – Charleston |
|
| |
|
Columbia |
|
Caris Healthcare – Columbia |
|
| |
|
Greenville |
|
Caris Healthcare – Greenville |
|
| |
|
Greenwood |
|
Caris Healthcare – Greenwood |
|
| |
|
Myrtle Beach |
|
Caris Healthcare – Myrtle Beach |
|
| |
|
Sumter |
|
Caris Healthcare – Sumter |
|
| |
|
|
|
|
|
| Tennessee |
|
Athens |
|
Caris Healthcare – Athens |
|
| |
|
Chattanooga |
|
Caris Healthcare – Chattanooga |
|
| |
|
Columbia |
|
Caris Healthcare – Columbia |
|
| |
|
Cookeville |
|
Caris Healthcare – Cookeville |
|
| |
|
Crossville |
|
Caris Healthcare – Crossville |
|
| |
|
Dickson |
|
Caris Healthcare – Dickson |
|
| |
|
Greeneville |
|
Caris Healthcare – Greeneville |
|
| |
|
Johnson City |
|
Caris Healthcare – Johnson City |
|
| |
|
Knoxville |
|
Caris Healthcare – Knoxville |
|
| |
|
Lenoir City |
|
Caris Healthcare – Lenoir City |
|
| |
|
Milan |
|
Caris Healthcare – Milan |
|
| |
|
Murfreesboro |
|
Caris Healthcare – Murfreesboro |
|
| |
|
Nashville |
|
Caris Healthcare – Nashville |
|
| |
|
Sevierville |
|
Caris Healthcare – Sevierville |
|
| |
|
Somerville |
|
Caris Healthcare – Somerville |
|
| |
|
Springfield |
|
Caris Healthcare – Springfield |
|
| |
|
Tullahoma |
|
Caris Healthcare – Tullahoma |
|
| |
|
|
|
|
|
| Virginia |
|
Big Stone Gap |
|
Caris Healthcare – Big Stone Gap |
|
| |
|
Bristol |
|
Caris Healthcare – Bristol |
|
Healthcare Facilities Leased to Others
The following table includes certain information regarding healthcare facilities which are owned by us and leased to others:
| Name of Facility |
|
Location |
|
No. of Beds |
| Skilled Nursing Facilities |
|
|
|
|
| Solaris HealthCare North Naples |
|
Naples, FL |
|
60 |
| Solaris HealthCare Coconut Creek |
|
Coconut Creek, FL |
|
120 |
| Solaris HealthCare Daytona |
|
Daytona Beach, FL |
|
73 |
| Solaris HealthCare Imperial |
|
Naples, FL |
|
113 |
| Solaris HealthCare Windermere |
|
Orlando, FL |
|
120 |
| Solaris HealthCare Charlotte Harbor |
|
Port Charlotte, FL |
|
180 |
| The Health Center at Standifer Place |
|
Chattanooga, TN |
|
444 |
| Solaris HealthCare Lake City |
|
Lake City, FL |
|
120 |
| Solaris HealthCare Pensacola |
|
Pensacola, FL |
|
180 |
| Assisted Living |
|
|
|
No. of Units |
| Solaris Senior Living Vero Beach |
|
Vero Beach, FL |
|
135 |
| Solaris Senior Living Merritt Island |
|
Merritt Island, FL |
|
95 |
| Solaris Senior Living Stuart |
|
Stuart, FL |
|
100 |
| Standifer Place Assisted Living |
|
Chattanooga, TN |
|
74 |
(1)Leased from NHI
(2) Knoxville Center for Behavioral Medicine is owned by separate limited liability companies. The Company owns 65% of the operations entity and owns 89% of the real estate entity.
(3)Ascension at Home St. Thomas is owned by a separate limited liability company. The Company owns 50% of the limited liability company.
| ITEM 3. |
LEGAL PROCEEDINGS |
General and Professional Liability Insurance and Lawsuits
The senior care industry has experienced increases in both the number of personal injury/wrongful death claims and in the severity of awards based upon alleged negligence by nursing facilities and their employees in providing care to residents. The Company has been, and continues to be, subject to claims and legal actions that arise in the ordinary course of business, including potential claims related to patient care and treatment. The defense of these lawsuits may result in significant legal costs, regardless of the outcome, and can result in large settlement amounts or damage awards.
As a result of the terms of our insurance policies and our use of a wholly-owned insurance company, we have retained significant self–insured risk with respect to general and professional liability. Additional insurance is purchased through third party providers that serve to supplement the coverage provided through our wholly-owned captive insurance company. We use independent actuaries to assist management in estimating our exposures for claims obligations (for both asserted and unasserted claims) related to exposures in excess of coverage limits, and we maintain reserves for these obligations. It is possible that claims against us could exceed our coverage limits and our reserves, which would have a material adverse effect on our financial position, results of operations and cash flows.
General Litigation
Qui Tam Litigation
United States of America, ex rel. Jennifer Cook and Sally Gaither v. Integrated Behavioral Health, Inc., NHC HealthCare/Moulton, LLC, et al., Case No. 2:20-CV-00877-AMM (N.D. Ala.) This is a qui tam case originally filed under seal on June 22, 2020. The United States declined intervention on March 1, 2021. Thereafter, the Plaintiff filed an amended Complaint against Dr. Sanja Malhotra, Integrated Behavioral Health, Inc. and other entities that Dr. Malhotra is alleged to own or in which he has a financial interest. The Complaint also named multiple skilled nursing facilities as Defendants, including NHC Healthcare/Moulton, LLC, an affiliate of National HealthCare Corporation. The Complaint alleges that nurse practitioners affiliated with Dr. Malhotra provided free services to the facilities in exchange for referrals to entities owned by or in which Dr. Malhotra had a financial interest in violation of the False Claims Act and Anti-Kickback Statute. NHC Healthcare/Moulton, LLC denies the allegations and is vigorously defending the claim. A motion to dismiss was filed on November 4, 2021. On January 28, 2022, the district court stayed this matter and administratively terminated the motion to dismiss pending the U.S. Supreme Court's review of a petition for certiorari filed in an unrelated matter but involving one of the legal arguments raised in the motion to dismiss. The U.S. Supreme Court recently denied the petition for certiorari in the unrelated matter. As a result, NHC Healthcare/Moulton, LLC’s motion to dismiss has been renewed and is now pending before the district court.
| ITEM 4. |
MINE SAFETY DISCLOSURES |
Not applicable.
PART II
| ITEM 5. |
MARKET FOR REGISTRANT'S COMMON EQUITY, RELATED STOCKHOLDER MATTERS, AND ISSUER PURCHASES OF EQUITY SECURITIES |
Market Information
Our common stock is listed and traded on the NYSE-American exchange under the symbol “NHC.” On December 31, 2022, NHC had approximately 10,750 stockholders, comprised of approximately 2,050 stockholders of record and an additional 8,700 stockholders indicated by security position listings.
Dividend Policy
We do not have a formal dividend policy, but we currently intend to continue to pay regular quarterly dividends to the holders of our common stock. The Company has paid a common dividend since 2004, although there can be no assurances that our quarterly dividends will be declared, paid or increased in the future.
Stock Repurchase Programs
In 2022, the Company purchased 148,547 shares of its common stock for a total cost of $9,903,000. The shares were funded from cash on hand and were cancelled and returned to the status of authorized but unissued.
Equity Compensation Plans
The following table sets forth information regarding our equity compensation plans:
| Plan Category |
|
Number of securities to be issued upon exercise of outstanding options, warrants and rights |
|
|
Weighted average exercise price of outstanding options, warrants and rights |
|
|
Number of securities remaining available for future issuance under equity compensation plans (excluding securities reflected in column (a)) |
|
| |
|
(a) |
|
|
(b) |
|
|
(c) |
|
| Equity compensation plans approved by security holders |
|
|
445,144 |
|
|
$ |
66.62 |
|
|
|
2,042,701 |
|
| Equity compensation plans not approved by security holders |
|
|
– |
|
|
|
– |
|
|
|
– |
|
| Total |
|
|
445,144 |
|
|
$ |
66.62 |
|
|
|
2,042,701 |
|
The following graph and chart compare the cumulative total stockholder return for the period from January 1, 2018 through December 31, 2022 on an investment of $100 in (i) NHC’s common stock, (ii) the Standard & Poor’s 500 Stock Index ("S&P 500 Index") and (iii) the Standard & Poor’s Health Care Index ("S&P Health Care Index"). Cumulative total stockholder return assumes the reinvestment of all dividends. Stock price performances shown in the graph are not necessarily indicative of future price performances.
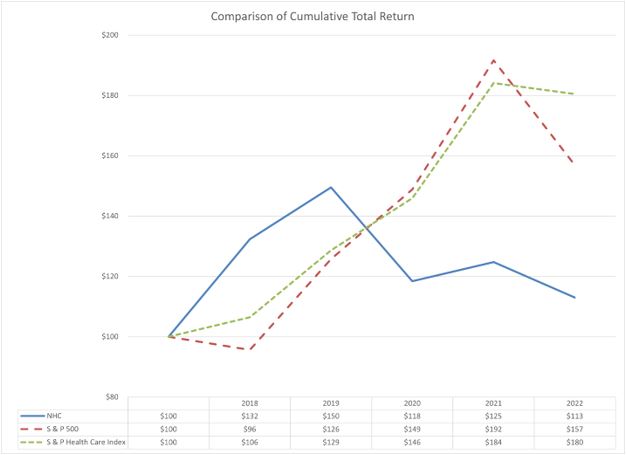
| ITEM 7. |
MANAGEMENT'S DISCUSSION AND ANALYSIS OF FINANCIAL CONDITION AND RESULTS OF OPERATIONS |
Overview
National HealthCare Corporation, which we also refer to as NHC or the Company, is a leading provider of post–acute care and senior health care services. At December 31, 2022, we operate or manage 68 skilled nursing facilities with 8,726 1icensed beds, 23 assisted living facilities with 1,181 units, five independent living facilities, three behavioral health hospitals, 35 homecare agencies, and 29 hospice agencies located in 8 states. In addition, we provide management services, accounting and financial services, and insurance services to third party operators of healthcare properties. We also own the real estate of 13 healthcare properties and lease these properties to third party operators.
Impact of COVID-19
In early March 2020, COVID-19, a disease caused by the novel strain of the coronavirus, was characterized as a pandemic by the World Health Organization. As a provider of healthcare services, we are significantly exposed to the public health and economic effects of the COVID-19 pandemic. NHC’s primary objective has remained the same throughout the COVID-19 pandemic: that is to protect the health and safety of our patients, residents, and partners (employees). We continue to follow all guidance from the Centers for Medicare and Medicaid Services (“CMS”), the Centers for Disease Control and Prevention (“CDC”), and state and local health departments to prevent the spread of the disease within our operations.
We began our first vaccination clinics in our skilled nursing facilities in December 2020. As the vaccination clinics progressed and as the vaccine became more accessible, we began to see a significant decline in COVID-19 cases among our operations, as well as a significant decrease in the adverse health events related to COVID. Despite the COVID-19 cases and adverse health events from COVID declining, our operating expenses have remained elevated with incentive compensation being paid to attract and retain frontline partners, as well as increased costs of personal protective equipment (“PPE”), sanitizers and cleaning supplies, and COVID-19 testing of our patients and partners. Despite the continued disruption of COVID-19 to our operations, our capital and financial resources, including our overall liquidity, remain strong. Our liquidity provides us with significant flexibility to maintain the strength of our balance sheet in periods of uncertainty or stress.
At this time, we are not able to quantify the impact that the COVID-19 pandemic will have on our future financial results. We have received and may continue to receive payments and advances from the various federal and state initiatives. These legislative initiatives have been beneficial to partially mitigate the impact of the COVID-19 pandemic on our results of operations and financial position to date.
Legislation and Government Stimulus Due to COVID-19
The U.S. government enacted several laws beginning in March 2020 designed to help the nation respond to the COVID-19 pandemic. The new laws impacted healthcare providers in a variety of ways, but the largest legislation from a monetary relief perspective is the CARES Act. Through the CARES Act, as well as the PPPCHE, the federal government allocated $178 billion to the Public Health and Social Services Emergency Fund, which is referred to as the Provider Relief Fund. The Provider Relief Fund is administered through grants and other mechanisms to skilled nursing providers, home health providers, hospitals, and other Medicare and Medicaid enrolled providers to cover unreimbursed health care related expenses or lost revenue attributable to the public health emergency resulting from COVID-19.
The Provider Relief Fund grants come with terms and condition certifications in which all providers are required to submit documents to ensure the funds are used for healthcare-related expenses or lost revenue attributable to COVID-19. The Company recorded $11,457,000, $63,360,000 and $47,505,000 of government stimulus income from the Provider Relief Funds for the years ended December 31, 2022, 2021 and 2020, respectively. The grant income was determined on a systemic basis in line with the recognition of specific expenses and lost revenues for which the grants are intended to compensate. The Company’s assessment of whether the terms and conditions for amounts received have been met for income recognition and the Company’s related income calculation considered all frequently asked questions and other interpretive guidance issued to date by HHS.
Additionally, as part of the CARES Act, the legislation included an expansion of the Medicare Accelerated and Advance Payment Program. In the second quarter of 2020, we received approximately $51,253,000 as part of this program. These funds began to be applied against claims for services provided to Medicare patients after approximately one year from the date we received the funds. The Company repaid $36,231,000 of the funds in 2021 and the remaining $15,022,000 of the funds in 2022.
The CARES Act and subsequent related legislation temporarily suspended Medicare sequestration beginning May 1, 2020 through March 31, 2022. The Medicare sequestration policy reduces fee-for-service Medicare payments by 2 percent. Beginning April 1, 2022, the sequestration reductions were 1% from April 1, 2022 through June 30, 2022. The full 2% reduction went back into effect July 1, 2022. The CARES Act extends the sequestration policy through 2030 in exchange for this temporary suspension, which the sequestration reduction for 2030 has been increased up to 3%.
The CARES Act also temporarily permitted employers to defer the deposit and payment of the employer’s portion of the social security taxes (6.2% of employee wages) that otherwise would have been due between March 27, 2020 and December 31, 2020. The provision requires that the deferred taxes be paid over a two-year period with half the amount required to be paid by December 31, 2021, and the other half by December 31, 2022. The Company paid $10,613,000 during the year ended December 31, 2021 and the remaining $10,545,000 during the year ended December 31, 2022.
Executive Summary
Earnings
To monitor our earnings, we have developed budgets and management reports to monitor labor, census, and the composition of revenues. Inflationary increases in our costs may cause net earnings from patient services to decline.
Occupancy
A primary area of management focus continues to be the rates of occupancy within our skilled nursing facilities. The overall census in owned and leased skilled nursing facilities for 2022 was 83.8% compared to 80.6% in 2021 and 83.6% in 2020.
Due to the pandemic, as well as the increased strain the pandemic has caused on America's healthcare labor shortage, the challenge of maintaining desirable patient census levels has been amplified. Management has undertaken a number of steps in order to best position our current and future operations. This includes working internally to examine and improve systems to be most responsive to referral sources and payors, as well as find creative initiatives to retain and attract qualified healthcare professionals. Additionally, NHC is in various stages of partnerships with hospital systems, payors, and other post–acute alliances to better position ourselves so we are an active participant in the delivery of post-acute healthcare services.
Quality of Patient Care
CMS introduced the Five-Star Quality Rating System to help consumers, their families and caregivers compare skilled nursing facilities more easily. The Five-Star Quality Rating System gives each skilled nursing operation a rating ranging between one and five stars in various categories (five stars being the best). The Company has always strived for patient-centered care and quality outcomes as precursors to outstanding financial performance.
In July 2022, CMS launched its enhanced Five-Star Quality Rating System which integrated weekend staffing rates for nurses and information on annual turnover among nurses and administrators. The tables below summarize NHC's overall performance in these Five-Star ratings versus the skilled nursing industry as of December 31, 2022:
| |
|
NHC Ratings |
|
|
Industry Ratings |
|
| Total number of skilled nursing facilities, end of period |
|
|
68 |
|
|
|
|
|
| Number of 4 and 5-star rated skilled nursing facilities |
|
|
42 |
|
|
|
|
|
| Percentage of 4 and 5-star rated skilled nursing facilities |
|
|
62% |
|
|
|
37% |
|
| Average rating for all skilled nursing facilities, end of period |
|
|
3.8 |
|
|
|
2.9 |
|
Development and Growth
We are undertaking to expand our post–acute and senior health care operations while protecting our existing operations and markets. The following table lists our recent construction and purchase activities.
| Type of Operation |
|
Description |
|
Size |
|
Location |
|
Placed in Service |
| Skilled Nursing |
|
Acquisition |
|
166 beds |
|
Knoxville, TN |
|
February 2020 |
| Assisted Living |
|
Bed Addition |
|
20 beds |
|
Gallatin, TN |
|
September 2020 |
| Skilled Nursing |
|
Bed Addition |
|
30 beds |
|
Kingsport, TN |
|
December 2020 |
| Hospice |
|
Acquisition |
|
28 agencies |
|
Various |
|
June 2021 |
| Homecare |
|
New Agency |
|
1 agency |
|
Anderson, SC |
|
January 2022 |
| Hospice |
|
New Agency |
|
1 agency |
|
Tullahoma, TN |
|
March 2022 |
| Behavioral Health Hospital |
|
New Facility |
|
64 beds |
|
Knoxville, TN |
|
April 2022 |
| Behavioral Health Hospital |
|
New Facility |
|
16 beds |
|
St. Louis, MO |
|
June 2022 |
Accrued Risk Reserves
Our accrued professional liability and workers’ compensation reserves totaled $102,469,000 and $98,048,000 at December 31, 2022 and 2021, respectively, and are a primary area of management focus. We have set aside restricted cash and restricted marketable securities to fund our professional liability and workers’ compensation reserves.
As to exposure for professional liability claims, we have developed performance measures to bring focus to the patient care issues most likely to produce professional liability exposure, including in–house acquired pressure ulcers, significant weight loss and numbers of falls. These programs for certification, which we regularly modify and improve, have produced measurable improvements in reducing these incidents. Our experience is that achieving goals in these patient care areas improves both patient and employee satisfaction.
Segment Reporting
The Company has two reportable operating segments: (1) inpatient services, which includes the operation of skilled nursing facilities, assisted and independent living facilities, and behavioral health hospitals; and (2) homecare and hospice services. These reportable operating segments are consistent with information used by the Company’s Chief Executive Officer, as chief operating decision maker (“CODM”), to assess performance and allocate resources. The Company also reports an “all other” category that includes revenues from rental income, management and accounting services fees, insurance services, and costs of the corporate office.
The Company’s CODM evaluates performance and allocates capital resources to each segment based on an operating model that is designed to improve the quality of patient care and profitability of the Company while enhancing long-term shareholder value. The CODM does not review assets by segment in his resource allocation and therefore, assets by segment are not disclosed below.
The following tables set forth the Company’s consolidated statements of operations by business segment (in thousands):
| |
|
Year Ended December 31, 2022 |
|
| |
|
Inpatient Services |
|
|
Homecare
and Hospice |
|
|
All Other |
|
|
Total |
|
| Revenues: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Net patient revenues |
|
$ |
900,231 |
|
|
$ |
128,854 |
|
|
$ |
– |
|
|
$ |
1,029,085 |
|
| Other revenues |
|
|
136 |
|
|
|
– |
|
|
|
45,060 |
|
|
|
45,196 |
|
| Government stimulus income |
|
|
11,457 |
|
|
|
– |
|
|
|
– |
|
|
|
11,457 |
|
| Net operating revenues and grant income |
|
|
911,824 |
|
|
|
128,854 |
|
|
|
45,060 |
|
|
|
1,085,738 |
|
| |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Costs and Expenses: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Salaries, wages and benefits |
|
|
580,707 |
|
|
|
77,688 |
|
|
|
27,774 |
|
|
|
686,169 |
|
| Other operating |
|
|
251,355 |
|
|
|
26,319 |
|
|
|
11,698 |
|
|
|
289,372 |
|
| Facility rent |
|
|
32,956 |
|
|
|
2,327 |
|
|
|
5,694 |
|
|
|
40,977 |
|
| Depreciation and amortization |
|
|
36,522 |
|
|
|
691 |
|
|
|
3,276 |
|
|
|
40,489 |
|
| Interest |
|
|
563 |
|
|
|
– |
|
|
|
– |
|
|
|
563 |
|
| Recovery of assets |
|
|
– |
|
|
|
– |
|
|
|
(3,728 |
) |
|
|
(3,728 |
) |
| Total costs and expenses |
|
|
902,103 |
|
|
|
107,025 |
|
|
|
44,714 |
|
|
|
1,053,842 |
|
| |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Income before non-operating income |
|
|
9,721 |
|
|
|
21,829 |
|
|
|
346 |
|
|
|
31,896 |
|
| Non-operating income |
|
|
– |
|
|
|
– |
|
|
|
11,141 |
|
|
|
11,141 |
|
| Unrealized losses on marketable equity securities |
|
|
– |
|
|
|
– |
|
|
|
(15,806 |
) |
|
|
(15,806 |
) |
| |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Income (loss) before income taxes |
|
$ |
9,721 |
|
|
$ |
21,829 |
|
|
$ |
(4,319 |
) |
|
$ |
27,231 |
|
| |
|
Year Ended December 31, 2021 |
|
| |
|
Inpatient Services |
|
|
Homecare
and Hospice |
|
|
All Other |
|
|
Total |
|
| Revenues: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Net patient revenues |
|
$ |
868,687 |
|
|
$ |
96,855 |
|
|
$ |
– |
|
|
$ |
965,542 |
|
| Other revenues |
|
|
386 |
|
|
|
– |
|
|
|
45,014 |
|
|
|
45,400 |
|
| Government stimulus income |
|
|
63,360 |
|
|
|
– |
|
|
|
– |
|
|
|
63,360 |
|
| Net operating revenues and grant income |
|
|
932,433 |
|
|
|
96,855 |
|
|
|
45,014 |
|
|
|
1,074,302 |
|
| |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Costs and Expenses: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Salaries, wages and benefits |
|
|
557,604 |
|
|
|
59,226 |
|
|
|
49,233 |
|
|
|
666,063 |
|
| Other operating |
|
|
238,354 |
|
|
|
16,053 |
|
|
|
12,347 |
|
|
|
266,754 |
|
| Facility rent |
|
|
32,819 |
|
|
|
2,064 |
|
|
|
5,935 |
|
|
|
40,818 |
|
| Depreciation and amortization |
|
|
36,890 |
|
|
|
443 |
|
|
|
3,339 |
|
|
|
40,672 |
|
| Interest |
|
|
845 |
|
|
|
– |
|
|
|
– |
|
|
|
845 |
|
| Impairment of assets |
|
|
4,497 |
|
|
|
– |
|
|
|
3,728 |
|
|
|
8,225 |
|
| Total costs and expenses |
|
|
871,009 |
|
|
|
77,786 |
|
|
|
74,582 |
|
|
|
1,023,377 |
|
| |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Income (loss) before non-operating income |
|
|
61,424 |
|
|
|
19,069 |
|
|
|
(29,568 |
) |
|
|
50,925 |
|
| Non-operating income |
|
|
– |
|
|
|
– |
|
|
|
17,774 |
|
|
|
17,774 |
|
| Gain on acquisition of equity method investment |
|
|
– |
|
|
|
– |
|
|
|
95,202 |
|
|
|
95,202 |
|
| Unrealized losses on marketable equity securities |
|
|
– |
|
|
|
– |
|
|
|
(13,863 |
) |
|
|
(13,863 |
) |
| |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Income before income taxes |
|
$ |
61,424 |
|
|
$ |
19,069 |
|
|
$ |
69,545 |
|
|
$ |
150,038 |
|
| |
|
Year Ended December 31, 2020 |
|
| |
|
Inpatient Services |
|
|
Homecare
and Hospice |
|
|
All Other |
|
|
Total |
|
| Revenues: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Net patient revenues |
|
$ |
879,693 |
|
|
$ |
52,102 |
|
|
$ |
– |
|
|
$ |
931,795 |
|
| Other revenues |
|
|
3,403 |
|
|
|
– |
|
|
|
45,514 |
|
|
|
48,917 |
|
| Government stimulus income |
|
|
47,505 |
|
|
|
– |
|
|
|
– |
|
|
|
47,505 |
|
| Net operating revenues and grant income |
|
|
930,601 |
|
|
|
52,102 |
|
|
|
45,514 |
|
|
|
1,028,217 |
|
| |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Costs and Expenses: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Salaries, wages and benefits |
|
|
546,188 |
|
|
|
37,377 |
|
|
|
37,427 |
|
|
|
620,992 |
|
| Other operating |
|
|
254,230 |
|
|
|
10,416 |
|
|
|
10,513 |
|
|
|
275,159 |
|
| Facility rent |
|
|
33,090 |
|
|
|
1,802 |
|
|
|
5,602 |
|
|
|
40,494 |
|
| Depreciation and amortization |
|
|
38,217 |
|
|
|
377 |
|
|
|
3,424 |
|
|
|
42,018 |
|
| Interest |
|
|
1,374 |
|
|
|
– |
|
|
|
25 |
|
|
|
1,399 |
|
| Total costs and expenses |
|
|
873,099 |
|
|
|
49,972 |
|
|
|
56,991 |
|
|
|
980,062 |
|
| |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Income (loss) before non-operating income |
|
|
57,502 |
|
|
|
2,130 |
|
|
|
(11,477 |
) |
|
|
48,155 |
|
| Non-operating income |
|
|
– |
|
|
|
– |
|
|
|
26,527 |
|
|
|
26,527 |
|
| Gain on acquisition of equity method investment |
|
|
– |
|
|
|
– |
|
|
|
1,707 |
|
|
|
1,707 |
|
| Unrealized losses on marketable equity securities |
|
|
– |
|
|
|
– |
|
|
|
(23,966 |
) |
|
|
(23,966 |
) |
| |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Income (loss) before income taxes |
|
$ |
57,502 |
|
|
$ |
2,130 |
|
|
$ |
(7,209 |
) |
|
$ |
52,423 |
|
Non-GAAP Financial Presentation
The Company is providing certain non-GAAP financial measures as the Company believes that these figures are helpful in allowing investors to more accurately assess the ongoing nature of the Company’s operations and measure the Company’s performance more consistently across periods. Therefore, the Company believes this information is meaningful in addition to the information contained in the GAAP presentation of financial information. The presentation of this additional non-GAAP financial information is not intended to be considered in isolation or as a substitute for the financial information prepared and presented in accordance with GAAP.
Specifically, the Company believes the presentation of non-GAAP financial information should exclude the following items: the unrealized gains or losses on our marketable equity securities, operating results for the newly constructed healthcare facilities not at full capacity, any gains on the acquisition of equity method investments, gains on the sale of healthcare facilities, stock-based compensation expense, and impairments or recoveries of long-lived assets and notes receivable.
The operating results for the start-up operations not at full capacity include the following: for the year ended December 31, 2022, included are operations that began from 2020 to 2022, which is two behavioral health hospitals, one hospice agency, and one homecare agency. For the year ended December 31, 2021, included are facilities that began operations from 2019 to 2021, which is one memory care facility and two behavioral health hospitals. For the year ended December 31, 2020, included are facilities that began operations from 2018 to 2020, which is one memory care facility.
The table below provides reconciliations of GAAP to non-GAAP items (dollars in thousands, except per share data):
| |
|
Year Ended December 31, |
|
| |
|
2022 |
|
|
2021 |
|
|
2020 |
|
| Net income attributable to National HealthCare Corporation |
|
$ |
22,445 |
|
|
$ |
138,590 |
|
|
$ |
41,871 |
|
| Non-GAAP adjustments: |
|
|
|
|
|
|
|
|
|
|
|
|
| Unrealized losses on marketable equity securities |
|
|
15,806 |
|
|
|
13,863 |
|
|
|
23,966 |
|
| Gain on sale of real estate/healthcare facilities |
|
|
– |
|
|
|
– |
|
|
|
(2,784 |
) |
| Gain on acquisition of equity method investment |
|
|
– |
|
|
|
(95,202 |
) |
|
|
(1,707 |
) |
| Stock-based compensation expense |
|
|
2,612 |
|
|
|
2,620 |
|
|
|
2,453 |
|
| Operating results for newly-opened operations not at full capacity |
|
|
5,416 |
|
|
|
922 |
|
|
|
602 |
|
| Impairment (recovery) of assets |
|
|
(3,728 |
) |
|
|
8,225 |
|
|
|
– |
|
| Income tax benefit on non-GAAP adjustments |
|
|
(5,228 |
) |
|
|
(6,373 |
) |
|
|
(5,858 |
) |
| Non-GAAP Net Income |
|
$ |
37,323 |
|
|
$ |
62,645 |
|
|
$ |
58,543 |
|
| |
|
|
|
|
|
|
|
|
|
|
|
|
| GAAP diluted earnings per share |
|
$ |
1.45 |
|
|
$ |
8.99 |
|
|
$ |
2.72 |
|
| Non-GAAP adjustments: |
|
|
|
|
|
|
|
|
|
|
|
|
| Unrealized losses on marketable equity securities |
|
|
0.76 |
|
|
|
0.67 |
|
|
|
1.15 |
|
| Gain on sale of real estate/healthcare facilities |
|
|
– |
|
|
|
– |
|
|
|
(0.13 |
) |
| Gain on acquisition of equity method investment |
|
|
– |
|
|
|
(6.16 |
) |
|
|
(0.08 |
) |
| Stock-based compensation expense |
|
|
0.13 |
|
|
|
0.13 |
|
|
|
0.12 |
|
| Operating results for newly-opened operations not at full capacity |
|
|
0.26 |
|
|
|
0.04 |
|
|
|
0.03 |
|
| Impairment (recovery) of assets |
|
|
(0.18 |
) |
|
|
0.39 |
|
|
|
– |
|
| Non-GAAP diluted earnings per share |
|
$ |
2.42 |
|
|
$ |
4.06 |
|
|
$ |
3.81 |
|
Results of Operations
The following table and discussion set forth items from the consolidated statements of operations as a percentage of net operating revenues and grant income for the years ended December 31, 2022, 2021 and 2020.
Percentage of Net Operating Revenues
| |
|
Year Ended December 31, |
|
| |
|
2022 |
|
|
2021 |
|
|
2020 |
|
| Revenues: |
|
|
|
|
|
|
|
|
|
|
|
|
| Net patient revenues |
|
|
94.8 |
% |
|
|
89.9 |
% |
|
|
90.6 |
% |
| Other revenues |
|
|
4.2 |
|
|
|
4.2 |
|
|
|
4.8 |
|
| Government stimulus income |
|
|
1.0 |
|
|
|
5.9 |
|
|
|
4.6 |
|
| Net operating revenues and grant income |
|
|
100.0 |
|
|
|
100.0 |
|
|
|
100.0 |
|
| Costs and Expenses: |
|
|
|
|
|
|
|
|
|
|
|
|
| Salaries, wages and benefits |
|
|
63.2 |
|
|
|
62.0 |
|
|
|
60.4 |
|
| Other operating |
|
|
26.6 |
|
|
|
24.8 |
|
|
|
26.8 |
|
| Facility rent |
|
|
3.8 |
|
|
|
3.8 |
|
|
|
3.9 |
|
| Depreciation and amortization |
|
|
3.7 |
|
|
|
3.8 |
|
|
|
4.1 |
|
| Interest |
|
|
0.1 |
|
|
|
0.1 |
|
|
|
0.1 |
|
| Impairment (recovery) of assets |
|
|
(0.3 |
) |
|
|
0.8 |
|
|
|
– |
|
| Total costs and expenses |
|
|
97.1 |
|
|
|
95.3 |
|
|
|
95.3 |
|
| Income from operations |
|
|
2.9 |
|
|
|
4.7 |
|
|
|
4.7 |
|
| Non–operating income |
|
|
1.0 |
|
|
|
1.7 |
|
|
|
2.6 |
|
| Gain on acquisition of equity method investments |
|
|
– |
|
|
|
8.8 |
|
|
|
0.1 |
|
| Unrealized losses on marketable equity securities |
|
|
(1.4 |
) |
|
|
(1.3 |
) |
|
|
(2.3 |
) |
| Income before income taxes |
|
|
2.5 |
|
|
|
13.9 |
|
|
|
5.1 |
|
| Income tax provision |
|
|
(0.7 |
) |
|
|
(1.0 |
) |
|
|
(1.0 |
) |
| Net income |
|
|
1.8 |
|
|
|
12.9 |
|
|
|
4.1 |
|
| Net loss attributable to noncontrolling interest |
|
|
0.3 |
|
|
|
0.0 |
|
|
|
0.0 |
|
| Net income attributable to common stockholders of NHC |
|
|
2.1 |
% |
|
|
12.9 |
% |
|
|
4.1 |
% |
The following table sets forth the increase or (decrease) in certain items from the consolidated statements of operations as compared to the prior period (dollars in thousands).
Period to Period Increase (Decrease)
| |
|
2022 vs. 2021 |
|
|
2021 vs. 2020 |
|
| |
|
Amount |
|
|
Percent |
|
|
Amount |
|
|
Percent |
|
| Revenues: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Net patient revenues |
|
$ |
63,543 |
|
|
|
6.6 |
% |
|
$ |
33,747 |
|
|
|
3.6 |
% |
| Other revenues |
|
|
(204 |
) |
|
|
(0.4 |
) |
|
|
(3,517 |
) |
|
|
(7.2 |
) |
| Government stimulus income |
|
|
(51,903 |
) |
|
|
(81.9 |
) |
|
|
15,855 |
|
|
|
33.4 |
|
| Net operating revenues and grant income |
|
|
11,436 |
|
|
|
1.1 |
|
|
|
46,085 |
|
|
|
4.5 |
|
| Costs and Expenses: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Salaries, wages and benefits |
|
|
20,106 |
|
|
|
3.0 |
|
|
|
45,071 |
|
|
|
7.3 |
|
| Other operating |
|
|
22,618 |
|
|
|
8.5 |
|
|
|
(8,405 |
) |
|
|
(3.1 |
) |
| Facility rent |
|
|
159 |
|
|
|
0.4 |
|
|
|
324 |
|
|
|
0.8 |
|
| Depreciation and amortization |
|
|
(183 |
) |
|
|
(0.4 |
) |
|
|
(1,346 |
) |
|
|
(3.2 |
) |
| Interest |
|
|
(282 |
) |
|
|
(33.4 |
) |
|
|
(554 |
) |
|
|
(39.6 |
) |
| Impairment (recovery) of assets |
|
|
(11,953 |
) |
|
|
(145.3 |
) |
|
|
8,225 |
|
|
|
100.0 |
|
| Total costs and expenses |
|
|
30,465 |
|
|
|
3.0 |
|
|
|
43,315 |
|
|
|
4.4 |
|
| Income from operations |
|
|
(19,029 |
) |
|
|
(37.4 |
) |
|
|
2,770 |
|
|
|
5.8 |
|
| Non–operating income |
|
|
(6,633 |
) |
|
|
(37.3 |
) |
|
|
(8,753 |
) |
|
|
(33.0 |
) |
| Gain on acquisition of equity method investment |
|
|
(95,202 |
) |
|
|
(100.0 |
) |
|
|
93,495 |
|
|
|
5,477.2 |
|
| Unrealized losses on marketable equity securities |
|
|
(1,943 |
) |
|
|
(14.0 |
) |
|
|
10,103 |
|
|
|
42.2 |
|
| Income before income taxes |
|
|
(122,807 |
) |
|
|
(81.9 |
) |
|
|
97,615 |
|
|
|
186.2 |
|
| Income tax provision |
|
|
3,697 |
|
|
|
33.8 |
|
|
|
(518 |
) |
|
|
(5.0 |
) |
| Net income |
|
|
(119,110 |
) |
|
|
(85.6 |
) |
|
|
97,097 |
|
|
|
231.2 |
|
| Net income attributable to noncontrolling interest |
|
|
2,965 |
|
|
|
596.6 |
|
|
|
(378 |
) |
|
|
(317.6 |
) |
| Net income attributable to common stockholders of NHC |
|
$ |
(116,145 |
) |
|
|
(83.8 |
)% |
|
$ |
96,719 |
|
|
|
231.0 |
% |
2022 Compared to 2021
Results for the year ended December 31, 2022 compared to 2021 include a 1.1% increase in net operating revenues and grant income. The net operating revenues and grant income increase is primarily driven by the June 2021 acquisition of Caris hospice and the continued occupancy increase in our skilled nursing facilities. These increases were offset by the reduction in government stimulus income of $51.9 million for the year ended December 31, 2022 compared to 2021.
For the year ended December 31, 2022, GAAP net income attributable to NHC was $22,445,000 compared to net income of $138,590,000 for the same period in 2021. The large decrease in our reported GAAP net income for 2022 was primarily due to the $95.2 million gain recorded in 2021 from the acquisition of Caris. Excluding the gain on the Caris acquisition, as well as the unrealized losses in our marketable equity securities portfolio and the other non-GAAP adjustments, non-GAAP net income for the year ended December 31, 2022 was $37,323,000 compared to $62,645,000 for the year ended December 31, 2021. The decrease in adjusted net income for the year ended December 31, 2022 compared to 2021 is primarily due to the $51.9 million less government stimulus income recorded during the 2022 period. We also continue to incur inflationary wage pressures within all areas of our operations.
Net operating revenues and grant income
Net patient revenues totaled $1,029,085,000, an increase of $63,543,000, or 6.6%, compared to the prior year. Included in net patient revenues for the year ended December 31, 2022 and 2021, respectively, is $19,442,000 and $20,482,000 of COVID-19 supplemental Medicaid payments that were received to help mitigate the incremental costs in fighting the public health emergency.
The overall average census in owned and leased skilled nursing facilities for 2022 was 83.8% compared to 80.6% in 2021. The composite skilled nursing facility per diem increased 2.3% in 2022 compared to 2021. Medicare and managed care per diem rates increased 2.3% and 6.0%, respectively, in 2022 compared to 2021. Medicaid and private pay per diem rates increased 3.0% and 4.7%, respectively, in 2022 compared to 2021.
In June 2021, the Company acquired the remaining ownership interest in Caris, which resulted in net patient revenues increasing $31,566,000 for the year ended December 31, 2022 compared to the prior year. In September 2022, the Company transferred the operations of seven skilled nursing facilities located in Massachusetts and New Hampshire resulting in net patient revenues decreasing $18,732,000 for the year ended December 31, 2022 compared to the prior year.
Other revenues in 2022 were $45,196,000, a decrease of $204,000, or 0.4%, as further detailed in Note 4 to our consolidated financial statements.
For the years ended December 31, 2022 and 2021, respectively, we recorded $11,457,000 and $63,360,000 in government stimulus income related to funds received from the CARES Act Provider Relief Fund.
Total costs and expenses
Total costs and expenses for 2022 increased $30,465,000, or 3.0%, to $1,053,842,000 from $1,023,377,000 in 2021.
Salaries, wages, and benefits increased $20,106,000, or 3.0%, to $686,169,000 from $666,063,000. Salaries, wages, and benefits as a percentage of net operating revenues and grant income was 63.2% compared to 62.0% for the years ended December 31, 2022 and 2021, respectively. Our Caris acquisition in June 2021 increased salaries, wages, and benefits $19,040,000 for the year ended December 31, 2022 compared to 2021. We continue to face workforce and labor shortages within all of our operations, which increases wage pressure in regards to retaining and attracting qualified healthcare partners (employees). The labor and workforce challenges have resulted in us contracting with agency nurse staffing companies. The agency nurse staffing companies charge inflated hourly rates; therefore, we are working diligently to find solutions to reduce and eliminate the agency nurse staffing within our healthcare operations. For the year ended December 31, 2022, our agency nurse staffing expenses were $68,875,000 compared to $36,391,000 for the 2021 year. In September 2022, the Company transferred the operations of seven skilled nursing facilities located in Massachusetts and New Hampshire resulting in salaries, wages, and benefits decreasing $18,053,000 for the year ended December 31, 2022 compared to the prior year.
Other operating expenses increased $22,618,000, or 8.5%, to $289,372,000 for the year ended December 31, 2022 compared to $266,754,000 for the prior year. Other operating expenses as a percentage of net operating revenues and grant income was 26.7% and 24.8% for the years ended December 31, 2022 and 2021, respectively. Our Caris acquisition increased other operating expenses $10,190,000 for the year ended December 31, 2022 compared to the prior year. The transfer of the operations of the seven skilled nursing facilities located in Massachusetts and New Hampshire, as noted above, resulted in other operating expenses decreasing $6,859,000 for the year ended December 31, 2022 compared to the prior year. We incurred increased expenses from our professional liability actuarial report in the fourth quarter of 2022 compared to the prior year of $3,284,000. We also continue to face inflationary pressures in certain categories within other operating expenses as well, such as food/dietary supplies and drugs/pharmaceutical supplies.
Facility rent expense increased $159,000, or 0.4%, to $40,977,000. Depreciation and amortization decreased 0.4% to $40,489,000. Interest expense decreased $282,000 to $563,000 in 2022 from $845,000 in 2021. At December 31, 2022, we have no outstanding long-term debt.
During 2022, we had a note receivable recovery of $3,728,000.
Other income
Non–operating income decreased by $6,633,000, or 37.3% to $11,141,000 compared to the prior year, as further detailed in Note 5 to our consolidated financial statements. The decrease in our non-operating income is due to the June 2021 acquisition of Caris. Prior to the June 2021 acquisition date, Caris was our most significant equity method investment with a 75.1% non-controlling ownership interest. From the respective acquisition date, Caris’ financial information is now included in the Company’s consolidated financial statements and is no longer accounted for as an equity method investment.
In June 2021, a gain of $95,202,000 was recorded on the acquisition of the remaining ownership interest of Caris. We previously held a noncontrolling interest in the partnership. Upon acquiring the remaining ownership interest in Caris, we valued the business and our previously held equity position (75.1%) based upon Caris' fair value at the acquisition date.
We recorded unrealized losses in the amount of $15,806,000 for the decrease in fair value of our marketable equity securities portfolio for the year ended December 31, 2022. The marketable equity securities portfolio consists mainly of publicly-traded healthcare REIT’s and other blue-chip public companies held within our insurance companies.
Income taxes
The income tax provision for 2022 is $7,254,000 (an effective income tax rate of 26.6%).
2021 Compared to 2020
Results for the year ended December 31, 2021 compared to 2020 include a 4.5% increase in net operating revenues and grant income and a 231.2% increase in net income attributable to NHC. For the year ended December 31, 2021, GAAP net income attributable to NHC was $138,590,000 compared to net income of $41,871,000 for the same period in 2020. The large increase in our reported GAAP 2021 net income compared to 2020 is primarily due to the $95.2 million gain recorded from the acquisition of Caris, a hospice provider. Excluding the gain on the Caris acquisition, as well as the unrealized losses in our marketable equity securities portfolio and the other non-GAAP adjustments, non-GAAP net income for the year ended December 31, 2021 was $62,645,000 compared to $58,543,000 for the year ended December 31, 2020.
Net operating revenues and grant income
Net patient revenues totaled $965,542,000, an increase of $33,747,000, or 3.6%, compared to the prior year. Included in net patient revenues for the year end December 31, 2021 and 2020, respectively, is $20,482,000 and $26,179,000 of COVID-19 supplemental Medicaid payments that were received to help mitigate the incremental costs in fighting the public health emergency.
The overall average census in owned and leased skilled nursing facilities for 2021 was 80.6% compared to 83.6% in 2020. The decline in census is due to COVID-19 and the lack of new admissions from our acute care providers and referral partners, and the difficult workforce and labor environment that has limited our admissions during phases of 2021. The composite skilled nursing facility per diem increased 2.4% in 2021 compared to 2020. Medicare and managed care per diem rates increased 2.0% and 1.3%, respectively, in 2021 compared to 2020. Medicaid and private pay per diem rates increased 2.2% and 2.4%, respectively, in 2021 compared to 2020.
In June 2021, the Company acquired the remaining ownership interest in Caris, which resulted in net patient revenues increasing $39,746,000 for the year ended December 31, 2021 compared to 2020. Our homecare operations had an increase in net patient revenues of approximately $5,007,000 for the year ended December 31, 2021 compared to 2020. In November 2020, the Company sold a skilled nursing facility located in Town & Country, Missouri. For the year ended December 31, 2021, the sale of this facility decreased net patient revenue by $7,323,000 compared to 2020.
Other revenues in 2021 were $45,400,000, a decrease of $3,517,000, or 7.2%, as further detailed in Note 4 of the consolidated financial statements.
For the years ended December 31, 2021 and 2020, respectively, we recorded $63,360,000 and $47,505,000 in government stimulus income related to funds received from the Provider Relief Fund. At December 31, 2021, we have not recognized as income $9,443,000 of Provider Relief Funds that are reflected in the current liability section of our consolidated balance sheet (provider relief funds) and used these funds in 2022. See Note 2 for additional information.
Total costs and expenses
Total costs and expenses for 2021 increased $43,315,000, or 4.4%, to $1,023,377,000 from $980,062,000 in 2020. In total, we incurred $21,555,000 and $47,674,000 of COVID-19 related expenses for the years ended December 31, 2021 and 2020, respectively. The COVID-19 related expenses primarily consisted of: (1) personal protective equipment and sanitizers/infection control supplies; (2) incentive compensation paid to our frontline partners/employees; and (3) COVID-19 testing of our patients and partners/employees. In 2021, we also incurred asset impairment expenses of $8,225,000 for the impairment and write-down of long-lived assets (leasehold improvements) and a credit impairment on a note receivable. Both of these impairment of assets items are due to the operating environment caused by COVID-19.
Salaries, wages and benefits, the largest operating costs of the company, increased $45,071,000, or 7.3%, to $666,063,000 from $620,992,000. Our salaries and wages were 62.0% and 60.4% of net operating revenues and grant income for 2021 and 2020, respectively. Our Caris acquisition in June 2021 increased salaries, wages, and benefits $20,754,000 for the year ended December 31, 2021 compared to 2020. We incurred COVID-related incentive pay (or combat pay) in the amount of $11,010,000 for the year ended December 31, 2021 compared to $15,224,000 for 2020. We continue to face tremendous workforce and labor shortages within all of our operations, which increases wage pressure and inflation in regards to retaining and attracting qualified healthcare partners (employees). With the workforce environment being so challenging, the largest expense increase from a labor standpoint is in our agency nurse staffing. For the year ended December 31, 2021, our agency nurse staffing expenses were $36,391,000 compared to $11,686,000 for the 2020 year.
Other operating expenses decreased $8,405,000, or 3.1%, to $266,754,000 for 2021 compared to $275,159,000 in 2020. These costs were 24.8% and 26.8% of net operating revenues and grant income for 2021 and 2020, respectively. For the years ended December 31, 2021 and 2020, respectively, we incurred $10,545,000 and $32,450,000 in COVID-19 related expenses in purchasing personal protective equipment, sanitizers and infection control supplies, and lab and testing supplies. Our Caris acquisition increased other operating expenses $8,368,000 for the year ended December 31, 2021 compared to 2020.
Facility rent expense decreased $324,000, or 0.8%, to $40,818,000. Depreciation and amortization decreased 3.2% to $40,672,000.
Interest expense decreased $554,000 to $845,000 in 2021 from $1,399,000 in 2020. At December 31, 2021, we have no outstanding long-term debt.
Other income
Non–operating income in 2021 decreased $8,753,000, or 33.0% to $17,744,000, as further detailed in Note 5 of the consolidated financial statements. The decrease is due to our June 2021 acquisition of Caris. From the respective acquisition date, we no longer record any equity in earnings from our Caris investment. Caris' financial information (revenues and expenses) is now included in the Company's consolidated financial statements.
In June 2021, a gain of $95,202,000 was recorded on the acquisition of the remaining ownership interest of Caris. We previously held a noncontrolling interest in the partnership. Upon acquiring the remaining ownership interest in Caris, we valued the business and our previously held equity position (75.1%) based upon Caris' fair value at the acquisition date. In February 2020, a gain of $1,707,000 was recorded on the acquisition of the remaining ownership interest of a 166-bed skilled nursing facility in Knoxville, Tennessee. We previously held a noncontrolling interest (25%) in the facility. Upon acquiring the remaining ownership interest, we valued our previously held equity position based upon the facility’s fair value.
We recorded unrealized losses in the amount of $13,863,000 for the decrease in fair value of our marketable equity securities portfolio for the year ended December 31, 2021.
Income taxes
The income tax provision for 2021 is $10,951,000 (an effective income tax rate of 7.3%). The income tax provision and effective tax rate for 2021 were favorably impacted by the nontaxable revaluation gain related to the Caris acquisition resulting in a benefit to the provision of $19,758,000 or 13.2% of income before income taxes. The income tax provision and effective tax rate for 2021 were also favorably impacted by the statute of limitation expirations resulting in a benefit to the provision of $1,901,000 or 1.3% of income before taxes in 2021.
Liquidity, Capital Resources and Financial Condition
Sources and Uses of Funds
Our primary sources of cash include revenues from the operations of our healthcare operations, management and accounting services, rental income, and investment income. Our primary uses of cash include salaries, wages and other operating costs of our healthcare operations, the cost of additions to and acquisitions of real property, facility rent expenses, and dividend distributions. These sources and uses of cash are reflected in our interim condensed consolidated statements of cash flows and are discussed in further detail below.
The following is a summary of our sources and uses of cash flows (dollars in thousands):
| |
|
Year Ended |
|
|
One Year Change |
|
|
Year Ended |
|
|
One Year Change |
|
| |
|
12/31/22 |
|
|
12/31/21 |
|
|
$ |
|
|
% |
|
|
12/31/21 |
|
|
12/31/20 |
|
|
$ |
|
|
% |
|
| Cash, cash equivalents, restricted cash, and restricted cash equivalents at beginning of period |
|
$ |
119,743 |
|
|
$ |
158,502 |
|
|
$ |
(38,759 |
) |
|
|
(24.5 |
) |
|
$ |
158,502 |
|
|
$ |
61,010 |
|
|
$ |
97,492 |
|
|
|
159.8 |
|
| |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Cash provided by operating activities |
|
|
8,742 |
|
|
|
62,394 |
|
|
|
(53,652 |
) |
|
|
(86.0 |
) |
|
|
62,394 |
|
|
|
203,259 |
|
|
|
(140,865 |
) |
|
|
(69.3 |
) |
| |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Cash used in investing activities |
|
|
(5,978 |
) |
|
|
(65,889 |
) |
|
|
59,911 |
|
|
|
90.9 |
|
|
|
(65,889 |
) |
|
|
(63,878 |
) |
|
|
(2,011 |
) |
|
|
(3.1 |
) |
| |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Cash used in financing activities |
|
|
(47,642 |
) |
|
|
(35,264 |
) |
|
|
(12,378 |
) |
|
|
(35.1 |
) |
|
|
(35,264 |
) |
|
|
(41,889 |
) |
|
|
6,625 |
|
|
|
15.8 |
|
| |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Cash, cash equivalents, restricted cash, and restricted cash equivalents at end of period |
|
$ |
74,865 |
|
|
$ |
119,743 |
|
|
$ |
(44,878 |
) |
|
|
(37.5 |
) |
|
$ |
119,743 |
|
|
$ |
158,502 |
|
|
$ |
(38,759 |
) |
|
|
(24.5 |
) |
Operating Activities
Net cash provided by operating activities for the year ended December 31, 2022 was $8,742,000 as compared to $62,394,000 and $203,259,000 for the years ended December 31, 2021 and 2020, respectively. Cash provided by operating activities consisted of net income of $19,977,000 and adjustments for non–cash items of $60,697,000. There was cash used for working capital in the amount of $73,697,000 for the year ended December 31, 2022 compared to 40,738,000 in 2021. We received cash distributions from our unconsolidated investments of $439,000 during the year ended December 31, 2022, compared to $6,314,000 in the prior year.
Included in the adjustments for non-cash items are depreciation expense, equity in earnings of unconsolidated investments, unrealized losses on our marketable equity securities, recovery of assets, deferred taxes, and stock compensation.
Investing Activities
Net cash used in investing activities totaled $5,978,000 for the year ended December 31, 2022, as compared to $65,889,000 and $63,878,000 for the years ended December 31, 2021 and 2020, respectively. Cash used for property and equipment additions was $30,200,000, $39,399,000, and $21,873,000 for the years ended December 31, 2022, 2021 and 2020, respectively. Proceeds from the sale of marketable securities, net of purchases, resulted in cash proceeds of $16,168,000 in 2022. In 2021, we had purchases of marketable securities, net of sales, that resulted in a net use of cash of $6,267,000. The Company collected notes receivable of $3,879,000 and $8,840,000 for the years ended December 31, 2022 and 2021, respectively. Additionally, the Company received proceeds from the sale of property and equipment of $4,175,000 for the year ended December 31, 2022. The acquisition of Caris hospice resulted in cash used of $28,713,000 in 2021.
Financing Activities
Net cash used in financing activities totaled $47,642,000, $35,264,000, and $41,889,000 for the years ended December 31, 2022, 2021, and 2020, respectively. Principal payments made under finance lease obligations was $4,695,000, $4,423,000, and $4,166,000 for the years ended December 31, 2022, 2021, and 2020, respectively. Dividends paid to common stockholders was $34,604,000, $32,030,000, and $31,921,000 for the years ended December 31, 2022, 2021 and 2020, respectively. Proceeds from the issuance of common stock totaled $2,114,000, $3,441,000, and $1,756,000 for 2022, 2021 and 2020, respectively. We repurchased common shares outstanding in the amount of $9,903,000, $836,000, and $53,000 for the years ended December 31, 2022, 2021, and 2020, respectively.
Short–term liquidity
We expect to meet our short–term liquidity requirements primarily from our cash flows from operating activities. In addition to cash flows from operations, our current cash on hand of $58,667,000 and unrestricted marketable securities of $123,922,000 are expected to be adequate to meet our contractual obligations, operating liquidity, and our growth and development plans in the next twelve months.
Long–term liquidity
We expect to meet our long–term liquidity requirements primarily from our cash flows from operating activities, our current cash on hand of $58,667,000, and unrestricted marketable securities of $123,922,000. We also have substantial value in our unencumbered real estate assets which could potentially be used as collateral in future borrowing opportunities. At December 31, 2022, we do not have any long-term debt.
Our ability to obtain long-term debt to meet our long–term contractual obligations and to finance our operating requirements, growth and development plans will depend upon our future performance, which will be affected by business, economic, financial and other factors, including potential changes in state and federal government payment rates for health care, customer demand, success of our marketing efforts, pressures from competitors, and the state of the economy, including the state of financial and credit markets.
Given the uncertainty in the rapidly changing market and economic conditions related to COVID-19, we will continue to evaluate the nature and extent of the impact to our business and financial position.
Contingencies
See Note 16 to the consolidated financial statements for additional information on pending litigation and other contingencies.
Guarantees
At December 31, 2022, we have no agreements to guarantee the debt obligations of other parties.
We have no outstanding letters of credit. We may or may not in the future elect to use financial derivative instruments to hedge interest rate exposure in the future. At December 31, 2022, we did not participate in any such financial instruments.
New Accounting Pronouncements
The Company did not adopt any new accounting standards during 2022.
Application of Critical Accounting Policies
The preparation of financial statements in conformity with accounting principles generally accepted in the United States of America requires us to make estimates and assumptions that affect the reported amounts of assets and liabilities and disclosure of contingent assets and liabilities at the date of the financial statements and the reported amounts of revenues and expenses during the reporting period. Actual results could differ from those estimates and cause our reported net income to vary significantly from period to period.
Our critical accounting policies that are both important to the portrayal of our financial condition and results and require our most difficult, subjective or complex judgments are as follows:
Net Patient Revenues and Accounts Receivable
Net patient revenues are derived from services rendered to patients for skilled and intermediate nursing, rehabilitation therapy, assisted living and independent living, home health care services and hospice services. Net patient revenue is reported at the amount that reflects the consideration to which the Company expects to be entitled in exchange for providing patient services. These amounts are due from patients, governmental programs, and other third-party payors, and include variable consideration for retroactive revenue adjustments due to settlement of audits, reviews, and investigations.
The Company recognizes revenue as its performance obligations are completed. Routine services are treated as a single performance obligation satisfied over time as services are rendered. These routine services represent a bundle of services that are not capable of being distinct. The performance obligations are satisfied over time as the patient simultaneously receives and consumes the benefits of the healthcare services provided. Additionally, there may be ancillary services which are not included in the daily rates for routine services, but instead are treated as separate performance obligations satisfied at a point in time when those services are rendered. Contract liabilities are recorded for payments the Company receives in which performance obligations have not been completed.
The Company determines the transaction price based on established billing rates reduced by explicit price concessions provided to third party payors. Explicit price concessions are based on contractual agreements and historical experience. The Company considers the patient's ability and intent to pay the amount of consideration upon admission. Credit losses are recorded as bad debt expense, which is included as a component of other operating expenses in the interim condensed consolidated statements of operations
Revenue Recognition – Third Party Payors
Medicare and Medicaid program revenues, as well as certain Managed Care program revenues, are subject to audit and retroactive adjustment by government representatives or their agents. Settlements with third-party payors for retroactive adjustments due to audits, reviews or investigations are considered variable consideration and are included in the determination of the estimated transaction price for providing patient care. These settlements are estimated based on the terms of the payment agreement with the payor, correspondence from the payor and the Company’s historical settlement activity, including an assessment to ensure that it is probable that a significant reversal in the amount of cumulative revenue recognized will not occur when the uncertainty associated with the retroactive adjustment is subsequently resolved.
In our opinion, adequate provision has been made for any adjustments that may result from these reviews. Any differences between our original estimates of reimbursements and subsequent revisions are reflected in operations in the period in which the revisions are made often due to final determination or the period of payment no longer being subject to audit or review.
Accrued Risk Reserves
We are self–insured for risks related to health insurance and have wholly–owned limited purpose insurance companies that insure risks related to workers’ compensation and general and professional liability insurance claims. The accrued risk reserves include a liability for reported claims and estimates for incurred but unreported claims. Our policy is to engage an external, independent actuary to assist in estimating our exposure for claims obligations (for both asserted and unasserted claims). We reassess our accrued risk reserves on a quarterly basis.
Professional liability remains an area of particular concern to us. The long-term care industry has seen an increase in personal injury/wrongful death claims based on alleged negligence by skilled nursing facilities and their employees in providing care to residents. The Company has been, and continues to be, subject to claims and legal actions that arise in the ordinary course of business, including potential claims related to patient care and treatment. A significant increase in the number of these claims, or an increase in the amounts due as a result of these claims could have a material adverse effect on our consolidated financial position, results of operations and cash flows. It is also possible that future events could cause us to make significant adjustments or revisions to these reserve estimates and cause our reported net income to vary significantly from period to period.
We are principally self-insured for incidents occurring in all centers owned or leased by us. The coverages include both primary policies and excess policies. In all years, settlements, if any, in excess of available insurance policy limits and our own reserves would be expensed by us.
| ITEM 7A. |
QUANTITATIVE AND QUALITATIVE DISCLOSURE ABOUT MARKET RISK |
Market risk represents the potential economic loss arising from adverse changes in the fair value of financial instruments. Currently, our exposure to market risk relates primarily to our fixed–income and equity portfolios. These investment portfolios are exposed primarily to, but not limited to, interest rate risk, credit risk, equity price risk, and concentration risk. We also have exposure to market risk that includes our cash and cash equivalents. The Company's senior management has established comprehensive risk management policies and procedures to manage these market risks.
Interest Rate Risk
The fair values of our fixed–income investments fluctuate in response to changes in market interest rates. Increases and decreases in prevailing interest rates generally translate into decreases and increases, respectively, in the fair values of those instruments. Additionally, the fair values of interest rate sensitive instruments may be affected by the creditworthiness of the issuer, prepayment options, the liquidity of the instrument and other general market conditions. At December 31, 2022, we have available for sale marketable debt securities in the amount of $142,647,000. The fixed income portfolio is comprised of investments with primarily short–term and intermediate–term maturities. The portfolio composition allows flexibility in reacting to fluctuations of interest rates. The fixed income portfolio allows our insurance company subsidiaries to achieve an adequate risk–adjusted return while maintaining sufficient liquidity to meet obligations.
Our cash and cash equivalents consist of highly liquid investments with a maturity of less than three months when purchased. As a result of the short–term nature of our cash instruments, a hypothetical 1% change in interest rates would have minimal impact on our future earnings and cash flows related to these instruments.
We do not currently use any derivative instruments to hedge our interest rate exposure. We have not used derivative instruments for trading purposes and the use of such instruments in the future would be subject to approvals by the Investment Committee of the Board of Directors.
Credit Risk
Credit risk is managed by diversifying the fixed income portfolio to avoid concentrations in any single industry group or issuer and by limiting investments in securities with lower credit ratings. Corporate debt securities and asset–backed securities comprise approximately 62% of the fair value of the fixed income portfolio. At December 31, 2022, the credit quality ratings for our fixed income portfolio consisted of the following investment and non-investment grades (as a percent of fair value): 41% AAA rated, 10% AA rated, 37% A rated, 10% BBB rated, and 2% BB rated.
Equity Price and Concentration Risk
Our marketable equity securities are recorded at their fair market value based on quoted market prices. Thus, there is exposure to equity price risk, which is the potential change in fair value due to a change in quoted market prices. At December 31, 2022, the fair value of our marketable equity securities is approximately $123,144,000. Our investment in NHI comprises approximately $85,152,000, or 69.2%, of the total fair value of our marketable equity securities. We manage our exposure to NHI by closely monitoring the financial condition, performance, and outlook of the company. Hypothetically, a 10% change in quoted market prices would result in a related increase or decrease in the fair value of our equity investments of approximately $12,314,000. At December 31, 2022, our equity securities had net unrealized gains of $68,642,000. Of the total unrealized gains in our marketable equity securities, approximately $60,418,000 is related to our investment in NHI.
| ITEM 8. |
FINANCIAL STATEMENTS AND SUPPLEMENTARY DATA |
REPORT OF INDEPENDENT REGISTERED PUBLIC ACCOUNTING FIRM
To the Stockholders and the Board of Directors of National HealthCare Corporation
Opinion on the Financial Statements
We have audited the accompanying consolidated balance sheets of National HealthCare Corporation (the Company) as of December 31, 2022 and 2021, the related consolidated statements of operations, comprehensive income, equity and cash flows for each of the three years in the period ended December 31, 2022, and the related notes and financial statement schedule listed in the Index at Item 15(a) (collectively referred to as the “consolidated financial statements”). In our opinion, the consolidated financial statements present fairly, in all material respects, the financial position of the Company at December 31, 2022 and 2021, and the results of its operations and its cash flows for each of the three years in the period ended December 31, 2022, in conformity with U.S. generally accepted accounting principles.
We also have audited, in accordance with the standards of the Public Company Accounting Oversight Board (United States) (PCAOB), the Company's internal control over financial reporting as of December 31, 2022, based on criteria established in Internal Control-Integrated Framework issued by the Committee of Sponsoring Organizations of the Treadway Commission (2013 framework), and our report dated February 17, 2023 expressed an unqualified opinion thereon.
Basis for Opinion
These financial statements are the responsibility of the Company’s management. Our responsibility is to express an opinion on the Company’s financial statements based on our audits. We are a public accounting firm registered with the PCAOB and are required to be independent with respect to the Company in accordance with the U.S. federal securities laws and the applicable rules and regulations of the Securities and Exchange Commission and the PCAOB.
We conducted our audits in accordance with the standards of the PCAOB. Those standards require that we plan and perform the audit to obtain reasonable assurance about whether the financial statements are free of material misstatement, whether due to error or fraud. Our audits included performing procedures to assess the risks of material misstatement of the financial statements, whether due to error or fraud, and performing procedures that respond to those risks. Such procedures included examining, on a test basis, evidence regarding the amounts and disclosures in the financial statements. Our audits also included evaluating the accounting principles used and significant estimates made by management, as well as evaluating the overall presentation of the financial statements. We believe that our audits provide a reasonable basis for our opinion.
Critical Audit Matter
The critical audit matter communicated below is a matter arising from the current period audit of the consolidated financial statements that was communicated or required to be communicated to the audit committee and that: (1) relates to accounts or disclosures that are material to the financial statements and (2) involved our especially challenging, subjective or complex judgments. The communication of the critical audit matter does not alter in any way our opinion on the consolidated financial statements, taken as a whole, and we are not, by communicating the critical audit matter below, providing a separate opinion on the critical audit matter or on the accounts or disclosures to which it relates.
| | | Estimation of Professional Liability Claims Reserves |
| Description of the Matter | | The Company’s accrued risk reserves totaled $102,469,000 as of December 31, 2022. As described in Note 16 to the consolidated financial statements, the accrued risk reserves include professional liability claims reserves for unpaid reported professional liability claims and estimates for incurred but unreported claims. The Company’s policy with respect to the professional liability claims reserves is to use an actuary to assist management in estimating the exposure for claims obligations (for both asserted and unasserted claims). Auditing management’s professional liability claims reserves was complex and highly judgmental due to the significant estimation required in determining the reserves, particularly the assumptions of the severity of asserted claims and the quantity and severity of unknown claims. |
| How We Addressed the Matter in Our Audit | | We obtained an understanding, evaluated the design and tested the effectiveness of controls over the Company’s professional liability claims reserve determination, including controls over management’s review of the significant assumptions described above. For example, we tested controls over management’s review of the actuarial analysis, the significant actuarial assumptions and the data inputs provided to the actuary. To test the professional liability claims reserves, our audit procedures included, among others, testing the completeness and accuracy of the underlying claims data provided to the Company’s actuarial specialist, obtaining legal confirmation letters to evaluate the reserves recorded on significant litigated matters, and reviewing the Company's insurance contracts by policy year to assess the Company's self-insured retentions, deductibles, and coverage limits. In addition, we involved our actuarial specialists to assist in our evaluation of the methodologies applied by management's specialist and assessing the accuracy of the Company’s reserves. We also compared the reserves recorded to a range developed by our actuarial specialists based on independently selected assumptions. |
We have served as the Company's auditor since 2009.
Nashville, Tennessee
February 17, 2023
NATIONAL HEALTHCARE CORPORATION
Consolidated Statements of Operations
(in thousands, except share and per share amounts)
| |
|
Year Ended December 31, |
|
| |
|
2022 |
|
|
2021 |
|
|
2020 |
|
| |
|
|
|
|
|
|
|
|
|
|
|
|
| Revenues: |
|
|
|
|
|
|
|
|
|
|
|
|
| Net patient revenues |
|
$ |
1,029,085 |
|
|
$ |
965,542 |
|
|
$ |
931,795 |
|
| Other revenues |
|
|
45,196 |
|
|
|
45,400 |
|
|
|
48,917 |
|
| Government stimulus income |
|
|
11,457 |
|
|
|
63,360 |
|
|
|
47,505 |
|
| Net operating revenues and grant income |
|
|
1,085,738 |
|
|
|
1,074,302 |
|
|
|
1,028,217 |
|
| |
|
|
|
|
|
|
|
|
|
|
|
|
| Costs and expenses: |
|
|
|
|
|
|
|
|
|
|
|
|
| Salaries, wages and benefits |
|
|
686,169 |
|
|
|
666,063 |
|
|
|
620,992 |
|
| Other operating |
|
|
289,372 |
|
|
|
266,754 |
|
|
|
275,159 |
|
| Facility rent |
|
|
40,977 |
|
|
|
40,818 |
|
|
|
40,494 |
|
| Depreciation and amortization |
|
|
40,489 |
|
|
|
40,672 |
|
|
|
42,018 |
|
| Interest |
|
|
563 |
|
|
|
845 |
|
|
|
1,399 |
|
| Impairment (recovery) of assets |
|
|
(3,728 |
) |
|
|
8,225 |
|
|
|
– |
|
| Total costs and expenses |
|
|
1,053,842 |
|
|
|
1,023,377 |
|
|
|
980,062 |
|
| |
|
|
|
|
|
|
|
|
|
|
|
|
| Income from operations |
|
|
31,896 |
|
|
|
50,925 |
|
|
|
48,155 |
|
| |
|
|
|
|
|
|
|
|
|
|
|
|
| Other income: |
|
|
|
|
|
|
|
|
|
|
|
|
| Non-operating income |
|
|
11,141 |
|
|
|
17,774 |
|
|
|
26,527 |
|
| Gain on acquisitions of equity method investments |
|
|
– |
|
|
|
95,202 |
|
|
|
1,707 |
|
| Unrealized losses on marketable equity securities |
|
|
(15,806 |
) |
|
|
(13,863 |
) |
|
|
(23,966 |
) |
| |
|
|
|
|
|
|
|
|
|
|
|
|
| Income before income taxes |
|
|
27,231 |
|
|
|
150,038 |
|
|
|
52,423 |
|
| Income tax provision |
|
|
(7,254 |
) |
|
|
(10,951 |
) |
|
|
(10,433 |
) |
| Net income |
|
|
19,977 |
|
|
|
139,087 |
|
|
|
41,990 |
|
| Net (income) loss attributable to noncontrolling interest |
|
|
2,468 |
|
|
|
(497 |
) |
|
|
(119 |
) |
| |
|
|
|
|
|
|
|
|
|
|
|
|
| Net income attributable to National HealthCare Corporation |
|
$ |
22,445 |
|
|
$ |
138,590 |
|
|
$ |
41,871 |
|
| |
|
|
|
|
|
|
|
|
|
|
|
|
| Earnings per share attributable to National HealthCare Corporation stockholders: |
|
|
|
|
|
|
|
|
|
|
|
|
| Basic |
|
$ |
1.46 |
|
|
$ |
9.03 |
|
|
$ |
2.74 |
|
| Diluted |
|
$ |
1.45 |
|
|
$ |
8.99 |
|
|
$ |
2.72 |
|
| |
|
|
|
|
|
|
|
|
|
|
|
|
| Weighted average common shares outstanding: |
|
|
|
|
|
|
|
|
|
|
|
|
| Basic |
|
|
15,410,222 |
|
|
|
15,347,129 |
|
|
|
15,306,174 |
|
| Diluted |
|
|
15,447,211 |
|
|
|
15,416,716 |
|
|
|
15,369,523 |
|
| |
|
|
|
|
|
|
|
|
|
|
|
|
| Dividends declared per common share |
|
$ |
2.26 |
|
|
$ |
2.11 |
|
|
$ |
2.08 |
|
The accompanying notes to consolidated financial statements are an integral part of these consolidated statements.
NATIONAL HEALTHCARE CORPORATION
Consolidated Statements of Comprehensive Income
(in thousands)
| |
|
Year Ended December 31, |
|
| |
|
2022 |
|
|
2021 |
|
|
2020 |
|
| |
|
|
|
|
|
|
|
|
|
|
|
|
| Net income |
|
$ |
19,977 |
|
|
$ |
139,087 |
|
|
$ |
41,990 |
|
| |
|
|
|
|
|
|
|
|
|
|
|
|
| Other comprehensive income (loss): |
|
|
|
|
|
|
|
|
|
|
|
|
| Unrealized gains (losses) on investments in marketable debt securities |
|
|
(12,946 |
) |
|
|
(4,171 |
) |
|
|
3,352 |
|
| Reclassification adjustment for realized gains on sale of marketable debt securities |
|
|
(129 |
) |
|
|
(214 |
) |
|
|
(195 |
) |
| Income tax (expense) benefit related to items of other comprehensive income (loss) |
|
|
1,938 |
|
|
|
933 |
|
|
|
(660 |
) |
| Other comprehensive income (loss), net of tax |
|
|
(11,137 |
) |
|
|
(3,452 |
) |
|
|
2,497 |
|
| |
|
|
|
|
|
|
|
|
|
|
|
|
| Net (income) loss attributable to noncontrolling interest |
|
|
2,468 |
|
|
|
(497 |
) |
|
|
(119 |
) |
| |
|
|
|
|
|
|
|
|
|
|
|
|
| Comprehensive income attributable to National HealthCare Corporation |
|
$ |
11,308 |
|
|
$ |
135,138 |
|
|
$ |
44,368 |
|
The accompanying notes to consolidated financial statements are an integral part of these consolidated statements.
NATIONAL HEALTHCARE CORPORATION
Consolidated Balance Sheets
(in thousands)
| | | December 31, | |
| | | 2022 | | | 2021 | |
| Assets | | | | | | | | |
| Current Assets: | | | | | | | | |
| Cash and cash equivalents | | $ | 58,667 | | | $ | 107,607 | |
| Restricted cash and cash equivalents, current portion | | | 15,121 | | | | 10,407 | |
| Marketable equity securities | | | 100,786 | | | | 113,108 | |
| Marketable debt securities | | | 23,136 | | | | 35,310 | |
| Restricted marketable equity securities | | | 22,358 | | | | 26,958 | |
| Restricted marketable debt securities, current portion | | | 16,244 | | | | 20,727 | |
| Accounts receivable | | | 99,986 | | | | 96,124 | |
| Inventories | | | 7,088 | | | | 8,582 | |
| Prepaid expenses and other assets | | | 10,244 | | | | 7,362 | |
| Notes receivable | | | 302 | | | | 453 | |
| Total current assets | | | 353,932 | | | | 426,638 | |
| | | | | | | | | |
| Property and Equipment: | | | | | | | | |
| Property and equipment, at cost | | | 1,081,219 | | | | 1,064,337 | |
| Accumulated depreciation and amortization | | | (574,687 | ) | | | (543,341 | ) |
| Net property and equipment | | | 506,532 | | | | 520,996 | |
| | | | | | | | | |
| Other Assets: | | | | | | | | |
| Restricted cash and cash equivalents, less current portion | | | 1,077 | | | | 1,729 | |
| Restricted marketable debt securities, less current portion | | | 103,267 | | | | 116,063 | |
| Deposits and other assets | | | 12,728 | | | | 4,499 | |
| Operating lease – right-of-use assets | | | 120,521 | | | | 156,116 | |
| Goodwill | | | 168,295 | | | | 168,295 | |
| Intangible assets | | | 7,038 | | | | 7,038 | |
| Investments in unconsolidated companies | | | 2,060 | | | | 2,022 | |
| Total other assets | | | 414,986 | | | | 455,762 | |
| Total assets | | $ | 1,275,450 | | | $ | 1,403,396 | |
The accompanying notes to consolidated financial statements are an integral part of these consolidated statements.
NATIONAL HEALTHCARE CORPORATION
Consolidated Balance Sheets
(in thousands, except share and per share amounts)
| | | December 31, | |
| | | 2022 | | | 2021 | |
| Liabilities and Equity | | | | | | | | |
| Current Liabilities: | | | | | | | | |
| Trade accounts payable | | $ | 16,958 | | | $ | 22,488 | |
| Finance lease obligations, current portion | | | 4,985 | | | | 4,695 | |
| Operating lease liabilities, current portion | | | 29,075 | | | | 27,574 | |
| Accrued payroll | | | 72,510 | | | | 106,698 | |
| Amounts due to third party payors | | | 16,631 | | | | 17,595 | |
| Accrued risk reserves, current portion | | | 31,365 | | | | 31,134 | |
| Other current liabilities | | | 17,615 | | | | 20,059 | |
| Provider relief funds | | | - | | | | 9,443 | |
| Contract liabilities | | | - | | | | 15,022 | |
| Dividends payable | | | 8,748 | | | | 8,493 | |
| Total current liabilities | | | 197,887 | | | | 263,201 | |
| | | | | | | | | |
| Finance lease obligations, less current portion | | | 860 | | | | 5,845 | |
| Operating lease liabilities, less current portion | | | 91,016 | | | | 128,542 | |
| Accrued risk reserves, less current portion | | | 71,104 | | | | 66,914 | |
| Refundable entrance fees | | | 6,207 | | | | 7,011 | |
| Deferred income taxes | | | 10,909 | | | | 6,852 | |
| Other noncurrent liabilities | | | 19,953 | | | | 16,571 | |
| Total liabilities | | | 397,936 | | | | 494,936 | |
| | | | | | | | | |
| Equity: | | | | | | | | |
| Common stock, $.01 par value; 45,000,000 shares authorized; 15,357,746 and 15,452,033 shares, respectively, issued and outstanding | | | 153 | | | | 154 | |
| Capital in excess of par value | | | 226,991 | | | | 232,167 | |
| Retained earnings | | | 656,664 | | | | 669,078 | |
| Accumulated other comprehensive income (loss) | | | (9,532 | ) | | | 1,605 | |
| Total National HealthCare Corporation stockholders’ equity | | | 874,276 | | | | 903,004 | |
| Noncontrolling interest | | | 3,238 | | | | 5,456 | |
| Total equity | | | 877,514 | | | | 908,460 | |
| Total liabilities and equity | | $ | 1,275,450 | | | $ | 1,403,396 | |
The accompanying notes to consolidated financial statements are an integral part of these consolidated statements.
NATIONAL HEALTHCARE CORPORATION
Consolidated Statements of Cash Flows
(in thousands)
| | | Year Ended December 31, | |
| | | 2022 | | | 2021 | | | 2020 | |
| | | | | | | | | | | | | |
| Cash Flows From Operating Activities: | | | | | | | | | | | | |
| Net income | | $ | 19,977 | | | $ | 139,087 | | | $ | 41,990 | |
| Adjustments to reconcile net income to net cash provided by operating activities: | | | | | | | | | | | | |
| Depreciation and amortization | | | 40,489 | | | | 40,672 | | | | 42,018 | |
| Equity in earnings of unconsolidated investments | | | (477 | ) | | | (5,111 | ) | | | (12,342 | ) |
| Distributions from unconsolidated investments | | | 439 | | | | 6,314 | | | | 10,050 | |
| Unrealized losses on marketable equity securities | | | 15,806 | | | | 13,863 | | | | 23,966 | |
| (Gains) losses on sale of marketable securities | | | 1,326 | | | | (1,042 | ) | | | (195 | ) |
| Gains on acquisition of equity method investments | | | – | | | | (95,202 | ) | | | (1,707 | ) |
| Gain on sale of property and equipment | | | – | | | | – | | | | (2,784 | ) |
| Impairment (recovery) of assets | | | (3,728 | ) | | | 8,225 | | | | – | |
| Deferred income taxes | | | 5,995 | | | | (6,294 | ) | | | (10,593 | ) |
| Stock–based compensation | | | 2,612 | | | | 2,620 | | | | 2,453 | |
| Changes in operating assets and liabilities: | | | | | | | | | | | | |
| Accounts receivable | | | (3,862 | ) | | | 4,090 | | | | 4,529 | |
| Inventories | | | 1,494 | | | | 199 | | | | (1,249 | ) |
| Prepaid expenses and other assets | | | (11,111 | ) | | | (3,298 | ) | | | 4,727 | |
| Operating lease obligations | | | (430 | ) | | | – | | | | – | |
| Trade accounts payable | | | (5,530 | ) | | | (2,083 | ) | | | 1,429 | |
| Accrued payroll | | | (34,188 | ) | | | 17,292 | | | | 15,948 | |
| Amounts due to third party payors | | | (964 | ) | | | 649 | | | | 1,200 | |
| Accrued risk reserves | | | 4,421 | | | | (1,489 | ) | | | 3,454 | |
| Provider relief funds | | | (9,443 | ) | | | (6,625 | ) | | | 16,068 | |
| Contract liabilities | | | (15,022 | ) | | | (36,231 | ) | | | 51,253 | |
| Other current liabilities | | | (2,444 | ) | | | (1,380 | ) | | | 5,898 | |
| Other noncurrent liabilities | | | 3,382 | | | | (11,862 | ) | | | 7,146 | |
| Net cash provided by operating activities | | | 8,742 | | | | 62,394 | | | | 203,259 | |
| Cash Flows From Investing Activities: | | | | | | | | | | | | |
| Purchases of property and equipment | | | (30,200 | ) | | | (39,399 | ) | | | (21,873 | ) |
| Proceeds from the sale of property and equipment | | | 4,175 | | | | – | | | | 6,750 | |
| Investments in unconsolidated companies | | | – | | | | (350 | ) | | | (305 | ) |
| Acquisition of equity method investments | | | – | | | | (28,713 | ) | | | (6,648 | ) |
| Investments in notes receivable | | | – | | | | – | | | | (425 | ) |
| Collections of notes receivable | | | 3,879 | | | | 8,840 | | | | 2,483 | |
| Purchases of marketable securities | | | (33,793 | ) | | | (108,187 | ) | | | (84,854 | ) |
| Sale of marketable securities | | | 49,961 | | | | 101,920 | | | | 40,994 | |
| Net cash used in investing activities | | | (5,978 | ) | | | (65,889 | ) | | | (63,878 | ) |
| Cash Flows From Financing Activities: | | | | | | | | | | | | |
| Borrowings under credit facility | | | – | | | | – | | | | 40,000 | |
| Principal payments under credit facility | | | – | | | | – | | | | (50,000 | ) |
| Principal payments under finance lease obligations | | | (4,695 | ) | | | (4,423 | ) | | | (4,166 | ) |
| Dividends paid to common stockholders | | | (34,604 | ) | | | (32,030 | ) | | | (31,921 | ) |
| Issuance of common shares | | | 2,114 | | | | 3,441 | | | | 1,756 | |
| Repurchase of common shares | | | (9,903 | ) | | | (836 | ) | | | (53 | ) |
| Noncontrolling interest contributions (distributions) | | | 250 | | | | (964 | ) | | | 2,488 | |
| Entrance fee deposits (refunds) | | | (804 | ) | | | (452 | ) | | | 7 | |
| Net cash used in financing activities | | | (47,642 | ) | | | (35,264 | ) | | | (41,889 | ) |
| Net Increase (Decrease) in Cash, Cash Equivalents, Restricted Cash, and Restricted Cash Equivalents | | | (44,878 | ) | | | (38,759 | ) | | | 97,492 | |
| Cash, Cash Equivalents, Restricted Cash, and Restricted Cash Equivalents, Beginning of Period | | | 119,743 | | | | 158,502 | | | | 61,010 | |
| Cash, Cash Equivalents, Restricted Cash, and Restricted Cash Equivalents, End of Period | | $ | 74,865 | | | $ | 119,743 | | | $ | 158,502 | |
| | | | | | | | | | | | | |
| Balance Sheet Classifications: | | | | | | | | | | | | |
| Cash and cash equivalents | | $ | 58,667 | | | $ | 107,607 | | | $ | 147,093 | |
| Restricted cash and cash equivalents | | | 16,198 | | | | 12,136 | | | | 11,409 | |
| Total Cash, Cash Equivalents, Restricted Cash, and Restricted Cash Equivalents | | $ | 74,865 | | | $ | 119,743 | | | $ | 158,502 | |
NATIONAL HEALTHCARE CORPORATION
Consolidated Statements of Cash Flows
(continued, in thousands)
| |
|
Year Ended December 31, |
|
| |
|
2022 |
|
|
2021 |
|
|
2020 |
|
| Supplemental Information: |
|
|
|
|
|
|
|
|
|
|
|
|
| |
|
|
|
|
|
|
|
|
|
|
|
|
| Cash payments for interest |
|
$ |
493 |
|
|
$ |
845 |
|
|
$ |
1,425 |
|
| |
|
|
|
|
|
|
|
|
|
|
|
|
| Cash payments for income taxes |
|
|
8,765 |
|
|
|
22,881 |
|
|
|
16,524 |
|
| |
|
|
|
|
|
|
|
|
|
|
|
|
| Non-cash activities include: |
|
|
|
|
|
|
|
|
|
|
|
|
| Noncontrolling interest contribution of land |
|
|
– |
|
|
|
2,840 |
|
|
|
– |
|
The accompanying notes to consolidated financial statements are an integral part of these consolidated statements.
NATIONAL HEALTHCARE CORPORATION
Consolidated Statements of Equity
(in thousands, except for share and per share amounts)
| |
|
Common Stock |
|
|
Capital in Excess of |
|
|
Retained |
|
|
Accumulated Other Comprehensive |
|
|
Non- controlling |
|
|
Total |
|
| |
|
Shares |
|
|
Amount |
|
|
Par Value |
|
|
Earnings |
|
|
Income (Loss) |
|
|
Interest |
|
|
Equity |
|
| Balance at January 1, 2020 |
|
|
15,332,206 |
|
|
$ |
153 |
|
|
$ |
222,787 |
|
|
$ |
553,093 |
|
|
$ |
2,560 |
|
|
$ |
476 |
|
|
$ |
779,069 |
|
| Net income |
|
|
– |
|
|
|
– |
|
|
|
– |
|
|
|
41,871 |
|
|
|
– |
|
|
|
119 |
|
|
|
41,990 |
|
| Contributions attributable to noncontrolling interest |
|
|
– |
|
|
|
– |
|
|
|
– |
|
|
|
– |
|
|
|
– |
|
|
|
2,488 |
|
|
|
2,488 |
|
| Other comprehensive income |
|
|
– |
|
|
|
– |
|
|
|
– |
|
|
|
– |
|
|
|
2,497 |
|
|
|
– |
|
|
|
2,497 |
|
| Stock–based compensation |
|
|
– |
|
|
|
– |
|
|
|
2,453 |
|
|
|
– |
|
|
|
– |
|
|
|
– |
|
|
|
2,453 |
|
| Shares sold – options exercised |
|
|
38,336 |
|
|
|
– |
|
|
|
1,756 |
|
|
|
– |
|
|
|
– |
|
|
|
– |
|
|
|
1,756 |
|
| Repurchase of common shares |
|
|
(797 |
) |
|
|
– |
|
|
|
(53 |
) |
|
|
– |
|
|
|
– |
|
|
|
– |
|
|
|
(53 |
) |
| Dividends declared to common stockholders ($2.08 per share) |
|
|
– |
|
|
|
– |
|
|
|
– |
|
|
|
(31,940 |
) |
|
|
– |
|
|
|
– |
|
|
|
(31,940 |
) |
| Balance at January 1, 2021 |
|
|
15,369,745 |
|
|
$ |
153 |
|
|
$ |
226,943 |
|
|
$ |
563,024 |
|
|
$ |
5,057 |
|
|
$ |
3,083 |
|
|
$ |
798,260 |
|
| Net income |
|
|
– |
|
|
|
– |
|
|
|
– |
|
|
|
138,590 |
|
|
|
– |
|
|
|
497 |
|
|
|
139,087 |
|
| Contributions attributable to noncontrolling interest |
|
|
– |
|
|
|
– |
|
|
|
– |
|
|
|
– |
|
|
|
– |
|
|
|
1,876 |
|
|
|
1,876 |
|
| Other comprehensive loss |
|
|
– |
|
|
|
– |
|
|
|
|
|
|
|
– |
|
|
|
(3,452 |
) |
|
|
– |
|
|
|
(3,452 |
) |
| Stock–based compensation |
|
|
– |
|
|
|
– |
|
|
|
2,620 |
|
|
|
– |
|
|
|
– |
|
|
|
– |
|
|
|
2,620 |
|
| Shares sold – options exercised |
|
|
90,725 |
|
|
|
1 |
|
|
|
3,440 |
|
|
|
– |
|
|
|
– |
|
|
|
– |
|
|
|
3,441 |
|
| Repurchase of common shares |
|
|
(8,437 |
) |
|
|
– |
|
|
|
(836 |
) |
|
|
– |
|
|
|
– |
|
|
|
– |
|
|
|
(836 |
) |
| Dividends declared to common stockholders ($2.11 per share) |
|
|
– |
|
|
|
– |
|
|
|
– |
|
|
|
(32,536 |
) |
|
|
– |
|
|
|
– |
|
|
|
(32,536 |
) |
| Balance at January 1, 2022 |
|
|
15,452,033 |
|
|
$ |
154 |
|
|
$ |
232,167 |
|
|
$ |
669,078 |
|
|
$ |
1,605 |
|
|
$ |
5,456 |
|
|
$ |
908,460 |
|
| Net income (loss) |
|
|
– |
|
|
|
– |
|
|
|
– |
|
|
|
22,445 |
|
|
|
– |
|
|
|
(2,468 |
) |
|
|
19,977 |
|
| Contributions attributable to noncontrolling interest |
|
|
– |
|
|
|
– |
|
|
|
– |
|
|
|
– |
|
|
|
– |
|
|
|
250 |
|
|
|
250 |
|
| Other comprehensive loss |
|
|
– |
|
|
|
– |
|
|
|
– |
|
|
|
– |
|
|
|
(11,137 |
) |
|
|
– |
|
|
|
(11,137 |
) |
| Stock–based compensation |
|
|
– |
|
|
|
– |
|
|
|
2,612 |
|
|
|
– |
|
|
|
– |
|
|
|
– |
|
|
|
2,612 |
|
| Shares sold – options exercised |
|
|
54,260 |
|
|
|
– |
|
|
|
2,114 |
|
|
|
– |
|
|
|
– |
|
|
|
– |
|
|
|
2,114 |
|
| Repurchase of common shares |
|
|
(148,547 |
) |
|
|
(1 |
) |
|
|
(9,902 |
) |
|
|
– |
|
|
|
– |
|
|
|
– |
|
|
|
(9,903 |
) |
| Dividends declared to common stockholders ($2.26 per share) |
|
|
– |
|
|
|
– |
|
|
|
– |
|
|
|
(34,859 |
) |
|
|
– |
|
|
|
– |
|
|
|
(34,859 |
) |
| Balance at December 31, 2022 |
|
|
15,357,746 |
|
|
$ |
153 |
|
|
$ |
226,991 |
|
|
$ |
656,664 |
|
|
$ |
(9,532 |
) |
|
$ |
3,238 |
|
|
$ |
877,514 |
|
The accompanying notes to consolidated financial statements are an integral part of these consolidated statements.
Notes to Consolidated Financial Statements
Note 1 – Summary of Significant Accounting Policies
Nature of Operations
National HealthCare Corporation ("NHC" or "the Company") operates, manages or provides services to skilled nursing facilities, assisted living facilities, independent living facilities, home health care agencies, hospice agencies, and behavioral health hospitals located in 8 Southeastern and Midwestern states in the United States. The most significant part of our business relates to skilled and intermediate nursing care settings in which we also provide assisted living and retirement services, rehabilitative therapy services, memory and Alzheimer's care services, home health and hospice services, and behavioral health services. In addition, we provide insurance services, management and accounting services, and we lease properties to operators of skilled nursing and assisted living facilities. The health care environment has continually undergone changes with regard to federal and state reimbursement programs and other payor sources, compliance regulations, competition among other health care providers and patient care litigation issues. We continually monitor these industry developments as well as other factors that affect our business.
Principles of Consolidation and Basis of Presentation
The consolidated financial statements, which are prepared in accordance with U.S. generally accepted accounting principles (“GAAP”), include our wholly owned and controlled subsidiaries and affiliates. All significant intercompany transactions and balances have been eliminated in consolidation. The Company presents noncontrolling interest within the equity section of its consolidated balance sheets. The Company presents the amount of consolidated net income that is attributable to NHC and the noncontrolling interest in its consolidated statements of operations.
Variable interest entities (“VIEs”) in which we have an interest have been consolidated when we have been identified as the primary beneficiary. Investments in ventures in which we have the ability to exercise significant influence but do not have control over are accounted for using the equity method. Equity method investments are initially recorded at cost and subsequently are adjusted for our share of the venture’s earnings or losses and cash distributions. Investments in entities in which we lack the ability to exercise significant influence are included in the consolidated financial statements at cost unless there has been a decline in the market value of our investment that is deemed to be other than temporary.
Use of Estimates
The preparation of financial statements in conformity with U.S. GAAP requires us to make estimates and assumptions that affect the reported amounts of assets and liabilities and disclosure of contingent assets and liabilities at the date of the financial statements and the reported amounts of revenues and expenses during the reporting period. Actual results could differ from those estimates and could cause our reported net income to vary significantly from period to period, including but not limited to, the potential future effects of the novel coronavirus (“COVID-19”).
Net Patient Revenues and Accounts Receivable
Net patient revenues are derived from services rendered to patients for skilled and intermediate nursing, rehabilitation therapy, assisted living and independent living, home health care services, hospice services, and behavioral health services. Net patient revenue is reported at the amount that reflects the consideration to which the Company expects to be entitled in exchange for providing patient services. These amounts are due from patients, governmental programs, and other third-party payors, and include variable consideration for retroactive revenue adjustments due to settlement of audits, reviews, and investigations.
The Company recognizes revenue as its performance obligations are completed. Routine services are treated as a single performance obligation satisfied over time as services are rendered. These routine services represent a bundle of services that are not capable of being distinct. The performance obligations are satisfied over time as the patient simultaneously receives and consumes the benefits of the healthcare services provided. Additionally, there may be ancillary services which are not included in the daily rates for routine services, but instead are treated as separate performance obligations satisfied at a point in time when those services are rendered. Contract liabilities are recorded for payments the Company receives in which performance obligations have not been completed.
The Company determines the transaction price based on established billing rates reduced by explicit price concessions provided to third party payors. Explicit price concessions are based on contractual agreements and historical experience. The Company considers the patient's ability and intent to pay the amount of consideration upon admission. Credit losses are recorded as bad debt expense, which is included as a component of other operating expenses in the consolidated statements of operations. Bad debt expense was $4,711,000, $3,886,000, and $3,339,000 for years ended December 31, 2022, 2021, and 2020, respectively. As of December 31, 2022, and 2021, the Company has recorded allowance for doubtful accounts of $6,246,000 and $6,411,000, respectively, as our best estimate of probable losses inherent in the accounts receivable balance.
Other Revenues
Other revenues include revenues from the provision of insurance services, management and accounting services to other long–term care providers, and rental income. Our insurance revenues consist of premiums that are generally paid in advance and then amortized into income over the policy period. We charge for management services based on a percentage of net revenues. We charge for accounting services based on a monthly fee or a fixed fee per bed of the healthcare center under contract. We record other revenues as the performance obligations are satisfied based on the terms of our contractual arrangements.
We recognize rental income based on the terms of our operating leases. Under certain of our leases, we receive variable rent, which is based on the increase in revenues of a lessee over a base year. We recognize variable rent annually or monthly, as applicable, when, based on the actual revenue of the lessee is earned.
Government Grants
We account for government grants in accordance with International Accounting Standard (“IAS”) 20, Accounting for Government Grants and Disclosure of Government Assistance, and as such, we recognize grant income on a systematic basis in line with the recognition of specific expenses and lost revenues for which the grants are intended to compensate.
Segment Reporting
In accordance with the provisions of Accounting Standards Codification ("ASC") 280, Segment Reporting, the Company is required to report financial and descriptive information about its reportable operating segments. The Company has two reportable operating segments: (1) inpatient services, which includes the operation of skilled nursing facilities, assisted and independent living facilities, and behavioral health hospitals, and (2) homecare and hospice services. The Company also reports an “all other” category that includes revenues from rental income, management and accounting services fees, insurance services, and costs of the corporate office. See Note 6 for further disclosure of the Company’s operating segments.
Other Operating Expenses
Other operating expenses include the costs of care and services that we provide to the residents of our facilities and the costs of maintaining our facilities. Our primary patient care costs include drugs, medical supplies, purchased professional services, food, and professional liability insurance and licensing fees. The primary facility costs include utilities and property insurance.
General and Administrative Costs
With the Company being a healthcare provider, the majority of our expenses are "cost of revenue" items. Costs that could be classified as "general and administrative" by the Company would include its corporate office costs, excluding stock-based compensation, which were $20,651,000, $20,160,000, and $19,934,000 for the years ended December 31, 2022, 2021, and 2020, respectively.
Cash and Cash Equivalents
Cash equivalents include highly liquid investments with an original maturity of three months or less when purchased.
Restricted Cash and Cash Equivalents and Restricted Marketable Securities
Restricted cash and cash equivalents and restricted marketable securities represent assets that are primarily held by our wholly owned limited purpose insurance companies for workers' compensation and professional liability claims.
Investments in Marketable Securities and Restricted Marketable Securities
Our investments in marketable equity securities are carried at fair value with the changes in unrealized gains and losses recognized in our results of operations at each measurement date. Our investments in marketable debt securities are classified as available for sale securities and carried at fair value with the unrealized gains and losses recognized through accumulated other comprehensive income at each measurement date. For available for sale debt securities in an unrealized loss position, we first assess whether we intend to sell, or it is more likely than not that we will be required to sell the security before recovery of the amortized cost basis. If either of the criteria regarding intent or requirement to sell is met, the security’s cost basis is written down to fair value through our results of operations. For debt securities that do not meet the aforementioned criteria, we evaluate whether the decline in fair value has resulted from credit losses or other factors. If a credit loss exists, the present value of cash flows expected to be collected from the security are compared to the cost basis of the security. If the present value of cash flows expected to be collected is less than the amortized cost basis, a credit loss exists and an allowance for credit losses is recorded for the credit loss, limited by the amount that the fair value is less than the amortized cost basis. Realized gains and losses from securities are recognized in results of operations upon disposition of the securities using the specific identification method on a trade date basis.
Inventories
Inventories consist generally of food and supplies and are valued at the lower of cost or market, with cost determined on a first–in, first–out (FIFO) basis.
Mortgage and Other Notes Receivable
In accordance with ASC Topic 310, Receivables, NHC evaluates the carrying values of its mortgage and other notes receivable on an instrument-by-instrument basis. On a quarterly basis, NHC reviews its notes receivable for recoverability when events or circumstances, including the non–receipt of contractual principal and interest payments, significant deteriorations of the financial condition of the borrower and significant adverse changes in general economic conditions, indicate that the carrying amount of the note receivable may not be recoverable. If necessary, impairment is measured as the amount by which the carrying amount exceeds the discounted cash flows expected to be received under the note receivable or, if foreclosure is probable, the fair value of the collateral securing the note receivable.
For the year ended December 31, 2022, the Company recorded a recovery of a note receivable of $3,728,000 due to the borrower paying off the note. For the year ended December 31, 2021, the Company recorded a credit loss provision for this same note receivable of $3,728,00 due to the financial instability of the borrower. The recovery and credit loss provision of the note receivable is recorded in the consolidated statements of operations under the line item “impairment (recovery) of assets”.
Property and Equipment
Property and equipment are recorded at cost. Depreciation is provided by the straight–line method over the expected useful lives of the assets estimated as follows: buildings and improvements, 20–40 years and equipment and furniture, 3–15 years. Leasehold improvements are amortized over periods that do not exceed the non–cancelable respective lease terms using the straight–line method.
Expenditures for repairs and maintenance are charged to expense as incurred. Betterments, which significantly extend the useful life, are capitalized. We remove the costs and related allowances for accumulated depreciation or amortization from the accounts for properties sold or retired, and any resulting gains or losses are included in income.
In accordance with ASC Topic 360, Property, Plant, and Equipment, we evaluate the recoverability of the carrying values of our properties on a property-by-property basis. We review our properties for recoverability when events or circumstances, including significant physical changes in the property, significant adverse changes in general economic conditions, and significant deteriorations of the underlying cash flows of the property, indicate that the carrying amount of the property may not be recoverable. The need to recognize impairment is based on estimated future undiscounted cash flows from a property over the remaining useful life compared to the carrying value of that property. If recognition of impairment is necessary, it is measured as the amount by which the carrying amount of the property exceeds the estimated fair value of the property. Management has evaluated long-lived assets and determined there were impairment charges of $0, $4,497,000, and $0 during the years ended December 31, 2022, 2021, and 2020, respectively. The 2021 impairment charges were recorded in the consolidated statements of operations under the line item “impairment of assets” and were due to the August 2022 exit of the seven skilled nursing facilities in Massachusetts and New Hampshire.
Business Combinations
We account for acquisitions using the acquisition method of accounting in accordance with ASC 805, Business Combinations. Acquisitions are accounted for as purchases and are included in our consolidated financial statements from their respective acquisition dates. Assets acquired and liabilities assumed, if any, are measured at fair value on the acquisition date using the appropriate valuation method. Goodwill generated from acquisitions is recognized for the excess of the purchase price over the fair value of tangible and identifiable intangible assets acquired and liabilities assumed. In determining the fair value of identifiable assets, we use various valuation techniques. These valuation methods require us to make estimates and assumptions surrounding projected revenues and costs, future growth, and discount rates.
Long-Term Leases
The Company’s lease portfolio primarily consists of finance and operating real estate leases for certain skilled nursing facilities, assisted and independent living facilities, homecare and hospice offices, and pharmacy warehouses. The original terms of the leases typically range from two to fifteen years. Several of the real estate leases include renewal options which vary in length and may not include specific rent renewal amounts. We determine if an arrangement is a lease at inception of a contract. We determine the lease term by assuming exercise of renewal options that are reasonably certain.
The Company records right-of-use assets and liabilities for non-cancelable real estate operating leases with original or remaining lease terms in excess of one year. Leases with a lease term of 12 months or less at inception are not recorded and are expensed on a straight-line basis over the lease term. We recognize lease components and non-lease components together and not as separate parts of a lease for real estate leases.
Operating lease right-of-use assets and liabilities are recorded at the present value of the lease payments over the lease term. The present value of the lease payments are discounted using the incremental borrowing rate associated with each lease. The variable components of the lease payment that fluctuate with the operations of a health facility are not included in determining the right-of-use assets and lease liabilities. Rather, these variable components are expensed as incurred.
Goodwill and Other Intangible Assets
Goodwill represents the excess of the purchase price over the fair value of identifiable net assets acquired in business combinations. Goodwill is not amortized but is subject to an annual impairment test. We perform our annual goodwill impairment assessment on the first day of the fourth quarter. Tests are performed more frequently if events occur, or circumstances change that would more likely than not reduce the fair value of the reporting unit below its carrying amount.
The Company’s indefinite-lived intangible assets consist of trade names and certificates of need and licenses. The Company reviews indefinite-lived intangible assets for impairment on an annual basis or more frequently if events or changes in circumstances indicate that the carrying amount of the intangible asset may not be recoverable.
Accrued Risk Reserves
We are principally self–insured for risks related to employee health insurance and utilize wholly owned limited purpose insurance companies for workers’ compensation and professional liability claims. Accrued risk reserves primarily represent the accrual for risks associated with employee health insurance, workers’ compensation and professional liability claims. The accrued risk reserves include a liability for unpaid reported claims and estimates for incurred but unreported claims. Our policy with respect to a significant portion of our workers’ compensation and professional and general liability claims is to use an actuary to assist management in estimating our exposure for claims obligation (for both asserted and unasserted claims). Our health insurance reserve is based on our known claims incurred and an estimate of incurred but unreported claims determined by our analysis of historical claims paid. We reassess our accrued risk reserves on a quarterly basis, with changes in estimated losses being recorded in the consolidated statements of operations in the period first identified.
Other Current Liabilities
Other current liabilities primarily represent accruals for current federal and state income taxes, real estate taxes and other current liabilities.
Continuing Care Contracts and Refundable Entrance Fees
We have one continuing care retirement center (“CCRC”) within our operations. Residents at this retirement center may enter into continuing care contracts with us. The contract provides that 10% of the resident entry fee becomes non–refundable upon occupancy, and the remaining refundable portion of the entry fee is calculated using the lessor of the price at which the apartment is re–assigned or 90% of the original entry fee, plus 40% of any appreciation if the apartment exceeds the original resident’s entry fee.
Non-refundable fees are included as a component of the transaction price and are amortized into revenue over the actuarially determined remaining life of the resident, which is the expected period of occupancy by the resident. We pay the refundable portion of our entry fees to residents when they relocate from our community and the apartment is re-occupied. Refundable entrance fees are not included as part of the transaction price and are classified as refundable entrance fees in the Company's consolidated balance sheets. The balances of refundable entrance fees as of December 31, 2022 and December 31, 2021 were $6,207,000 and $7,011,000, respectively.
We annually estimate the present value of the net cost of future services and the use of facilities to be provided to the current CCRC residents and compare that amount with the balance of non–refundable deferred revenue from entrance fees received. If the present value of the net cost of future services exceeds the related anticipated revenues, a liability is recorded (obligation to provide future services) with a corresponding charge to income. The obligation to provide future services is included in other noncurrent liabilities in the Company’s consolidated balance sheets. At December 31, 2022 and 2021, we have recorded a future service obligation in the amounts of $2,218,000 and $2,338,000, respectively.
Other Noncurrent Liabilities
Other noncurrent liabilities include reserves primarily related to various uncertain income tax positions, deferred revenue, and obligations to provide services to our CCRC residents. Deferred revenue includes the deferred gain on the sale of assets to National Health Corporation (“National”) and the non-refundable portion (10%) of CCRC entrance fees being amortized over the remaining life expectancies of the residents.
Income Taxes
We utilize ASC Topic 740, Income Taxes, which requires an asset and liability approach for financial accounting and reporting for income taxes. Under this guidance, deferred tax assets and liabilities are determined based upon differences between financial reporting and tax basis of assets and liabilities and are measured using the enacted tax laws that will be in effect when the differences are expected to reverse. The effect on deferred tax assets and liabilities of a change in tax rates is recognized in income in the period that includes the enactment date. See Note 13 for further discussion of our accounting for income taxes.
Also, under ASC Topic 740, Income Taxes, tax positions are evaluated for recognition using a more–likely–than–not threshold, and those tax positions requiring recognition are measured at the largest amount of tax benefit that is greater than 50 percent likely of being realized upon ultimate settlement with a taxing authority that has full knowledge of all relevant information. Liabilities for income tax matters include amounts for income taxes, applicable penalties, and interest thereon and are the result of the potential alternative interpretations of tax laws and the judgmental nature of the timing of recognition of taxable income.
Noncontrolling Interest
The noncontrolling interest in a subsidiary is presented within total equity in the Company’s consolidated balance sheets. The Company presents the noncontrolling interest and the amount of consolidated net income attributable to NHC in its consolidated statements of operations. The Company’s earnings per share is calculated based on net income attributable to NHC’s stockholders. The carrying amount of the noncontrolling interest is adjusted based on an allocation of subsidiary earnings based on ownership interest.
Stock–Based Compensation
Stock–based awards granted include stock options, restricted stock units, and stock purchased under our employee stock purchase plan. Stock–based compensation cost is measured at the grant date, based on the fair value of the awards, and is recognized as expense over the requisite service period only for those equity awards expected to vest.
The fair value of the restricted stock units is determined based on the stock price on the date of grant. We estimated the fair value of stock options and stock purchased under our employee stock purchase plan using the Black–Scholes model. This model utilizes the estimated fair value of common stock and requires that, at the date of grant, we use the expected term of the grant, the expected volatility of the price of our common stock, risk–free interest rates and expected dividend yield of our common stock. The fair value is amortized on a straight–line basis over the requisite service periods of the awards.
Comprehensive Income
ASC Topic 220, Comprehensive Income, requires that changes in the amounts of certain items, including unrealized gains and losses on marketable debt securities, be shown in the consolidated financial statements as comprehensive income. We report comprehensive income in the consolidated statements of comprehensive income and also in the consolidated statements of stockholders’ equity.
Concentration of Credit Risks
Our credit risks primarily relate to cash and cash equivalents, restricted cash and cash equivalents, accounts receivable, marketable securities, restricted marketable securities and notes receivable. Cash and cash equivalents are primarily held in bank accounts and overnight investments. Restricted cash and cash equivalents are primarily invested in commercial paper and certificates of deposit with financial institutions and other interest-bearing accounts. Accounts receivable consist primarily of amounts due from patients (funded through Medicare, Medicaid, other contractual programs and through private payors) and from other health care companies for management, accounting and other services. We perform continual credit evaluations of our clients and maintain appropriate allowances for doubtful accounts on any accounts receivable proving uncollectible, and continually monitor and adjust these allowances as necessary. Marketable securities and restricted marketable securities are held primarily in accounts with brokerage institutions. Notes receivable relate primarily to secured loans with health care facilities.
At any point in time we have funds in our operating accounts and restricted cash accounts that are with third party financial institutions. These balances in the U.S. may exceed the Federal Deposit Insurance Corporation (“FDIC”) insurance limits. While we monitor the cash balances in our operating accounts, these cash and restricted cash balances could be impacted if the underlying financial institutions fail or could be subject to other adverse conditions in the financial markets.
Our financial instruments, principally our notes receivable, are subject to the possibility of loss of the carrying values as a result of the failure of other parties to perform according to their contractual obligations. We obtain various collateral and other protective rights, and continually monitor these rights in order to reduce such possibilities of credit loss. We evaluate the need to provide reserves for potential credit losses on our financial instruments based on management's periodic review of the portfolio on an instrument-by-instrument basis.
Reclassifications
Certain accounts in the prior-year financial statements have been reclassified for comparative purposes to conform to the presentation in the current-year financial statements.
Note 2 – Coronavirus Pandemic ("COVID-19")
In early March 2020, COVID-19, a disease caused by the novel strain of the coronavirus, was characterized as a pandemic by the World Health Organization. The U.S. government enacted several laws beginning in March 2020 designed to help the nation respond to the COVID-19 pandemic. The laws impacted healthcare providers in a variety of ways, but the largest legislation from a monetary relief perspective is the CARES Act. Through the CARES Act, as well as the PPPCHE, the federal government allocated $178 billion to the Public Health and Social Services Emergency Fund, which is referred to as the Provider Relief Fund. The Provider Relief Fund is administered through grants and other mechanisms to skilled nursing providers, home health providers, hospitals, and other Medicare and Medicaid enrolled providers to cover unreimbursed health care related expenses or lost revenue attributable to the public health emergency resulting from COVID-19.
The Provider Relief Fund grants come with terms and condition certifications in which all providers are required to submit documents to ensure the funds are used for healthcare-related expenses or lost revenue attributable to COVID-19. The Company recorded $11,457,000, $63,360,000 and $47,505,000 of government stimulus income from the Provider Relief Funds for the years ended December 31, 2022, 2021 and 2020, respectively. The grant income was determined on a systemic basis in line with the recognition of specific expenses and lost revenues for which the grants are intended to compensate. The Company’s assessment of whether the terms and conditions for amounts received have been met for income recognition and the Company’s related income calculation considered all frequently asked questions and other interpretive guidance issued to date by the U.S. Department of Health and Human Services (“HHS”).
Additionally, as part of the CARES Act, the legislation included an expansion of the Medicare Accelerated and Advance Payment Program. The expanded Medicare Accelerated and Advance Payment Program is a streamlined version of existing policy that allows the Medicare Administrative Contractors (“MAC’s”) to issue up to three months of advance Medicare payments to help increase cash flow and liquidity to Medicare Part A and Part B providers in certain circumstances that include national emergencies. In the second quarter of 2020, we received approximately $51,253,000 as part of this program. These funds began to be applied against claims for services provided to Medicare patients after approximately one year from the date we received the funds. The Company repaid $36,231,000 of the funds in 2021 and the remaining $15,022,000 of the funds in 2022.
The CARES Act and subsequent related legislation temporarily suspended Medicare sequestration beginning May 1, 2020 through March 31, 2022. The Medicare sequestration policy reduces fee-for-service Medicare payments by 2 percent. Beginning April 1, 2022, the sequestration reductions were 1% from April 1, 2022 through June 30, 2022. The full 2% reduction went back into effect July 1, 2022. The CARES Act extends the sequestration policy through 2030 in exchange for this temporary suspension, which the sequestration reduction for 2030 has been increased up to 3%.
The CARES Act also temporarily permitted employers to defer the deposit and payment of the employer’s portion of the social security taxes (6.2% of employee wages) that otherwise would have been due between March 27, 2020 and December 31, 2020. The provision requires that the deferred taxes be paid over a two-year period with half the amount required to be paid by December 31, 2021, and the other half by December 31, 2022. The Company paid $10,613,000 during the year ended December 31, 2021 and the remaining $10,545,000 during the year ended December 31, 2022.
We have also received supplemental Medicaid payments from many of the states in which we operate to help mitigate the incremental costs resulting from the COVID-19 public health emergency. We have recorded $19,442,000, $20,482,000 and $26,179,000 in net patient revenues for these supplemental Medicaid payments for the years ended December 31, 2022, 2021 and 2020, respectively.
Note 3 – Net Patient Revenues
The Company disaggregates revenue from contracts with customers by service type and by payor.
Revenue by Service Type
The Company’s net patient services can generally be classified into the following two categories: (1) inpatient services, which includes the operation of skilled nursing facilities, assisted and independent living facilities, and behavioral health hospitals, and (2) homecare and hospice services (in thousands).
| | | Year Ended December 31, | |
| | | 2022 | | | 2021 | | | 2020 | |
| Inpatient services | | $ | 900,231 | | | $ | 868,687 | | | $ | 879,693 | |
| Homecare services | | | 128,854 | | | | 96,855 | | | | 52,102 | |
| Total net patient revenues | | $ | 1,029,085 | | | $ | 965,542 | | | $ | 931,795 | |
For inpatient and hospice services, revenue is recognized on a daily basis as each day represents a separate contract and performance obligation. For homecare, revenue is recognized when services are provided based on the number of days of service rendered in the period of care or on a per-visit basis. Typically, patients and third-party payors are billed monthly after services are performed or the patient is discharged, and payments are due based on contract terms.
As our performance obligations relate to contracts with a duration of one year or less, the Company is not required to disclose the aggregate amount of the transaction price allocated to performance obligations that are unsatisfied or partially unsatisfied at the end of the reporting period. The Company has minimal unsatisfied performance obligations at the end of the reporting period as our patients are typically under no obligation to remain admitted in our facilities or under our care. As the period between the time of service and time of payment is typically one year or less, the Company did not adjust for the effects of a significant financing component.
Revenue by Payor
Certain groups of patients receive funds to pay the cost of their care from a common source. The following table sets forth sources of net patient revenues for the periods indicated:
| | | Year Ended December 31, | |
| Source | | 2022 | | | 2021 | | | 2020 | |
| Medicare | | | 37% | | | | 36% | | | | 33% | |
| Managed Care | | | 10% | | | | 11% | | | | 11% | |
| Medicaid | | | 28% | | | | 29% | | | | 31% | |
| Private Pay and Other | | | 25% | | | | 24% | | | | 25% | |
| Total | | | 100% | | | | 100% | | | | 100% | |
Medicare covers skilled nursing services for beneficiaries who require nursing care and/or rehabilitation services following a hospitalization of at least three consecutive days (there is temporary relief from the three-day hospital stay during the COVID-19 emergency). For each eligible day a Medicare beneficiary is in a skilled nursing facility, Medicare pays the facility a daily payment, subject to adjustment for certain factors such as a wage index in the geographic area. The payment covers all services provided by the skilled nursing facility for the beneficiary that day, including room and board, nursing, therapy and drugs, as well as an estimate of capital–related costs to deliver those services.
For homecare services, Medicare pays based on the acuity level of the patient and based on periods of care. A period of care is defined as a length of care up to 30 days with multiple continuous periods allowed. The services covered by the payment include all disciplines of care, in addition to medical supplies, within the scope of the home health benefit.
For hospice services, Medicare pays a daily rate to cover the hospice’s costs for providing services included in the patient care plan. Medicare makes daily payments based on 1 of 4 levels of hospice care. All hospice care and services offered to patients and their families must follow an individualized written plan of care that meets the patient’s needs.
Our hospice service revenue is subject to certain limitations on payments from Medicare. We are subject to an inpatient cap limit and an overall Medicare payment cap for each provider number. We monitor these caps on a provider-by-provider basis and estimate amounts due back to Medicare if we estimate a cap has been exceeded. If applicable, we record these cap adjustments as a reduction to revenue.
Medicaid is operated by individual states with the financial participation of the federal government. The states in which we operate currently use prospective cost–based reimbursement systems. Under cost–based reimbursement systems, the skilled nursing facility is reimbursed for the reasonable direct and indirect allowable costs it incurred in a base year in providing routine resident care services as defined by the program.
Private pay, managed care, and other payment sources include commercial insurance, individual patient funds, managed care plans and the Veterans Administration. Private paying patients, private insurance carriers and the Veterans Administration generally pay based on the healthcare center's charges or specifically negotiated contracts. For private pay patients in skilled nursing, assisted living and independent living facilities, the Company bills for room and board charges, with the remittance being due on receipt of the statement and generally by the 10th day of the month the services are performed.
Certain managed care payors for homecare services pay on a per-visit basis. This revenue is recorded on an accrual basis based upon the date of services at amounts equal to its established or estimated per-visit rates.
57
Contract Liabilities
Included in the Company’s consolidated balance sheets are contract liabilities, which represent payments the Company receives in advance of services provided. As of December 31, 2022 and 2021, the Company has recorded $0 and $15,022,000, respectively, in contract liabilities related to receipts from the Medicare Accelerated and Advance Payment Program. Recoupment of the accelerated payments began in the second quarter of 2021.
A summary of the contract liabilities are follows (in thousands):
| Balance, January 1, 2021 | | $ | 51,253 | |
| Payments recouped | | | (36,231 | ) |
| Balance, December 31, 2021 | | | 15,022 | |
| Payments recouped | | | (15,022 | ) |
| Balance, December 31, 2022 | | $ | – | |
Third Party Payors
Laws and regulations governing the Medicare and Medicaid programs are complex and subject to interpretation. Noncompliance with such laws and regulations can be subject to regulatory actions including fines, penalties, and exclusion from the Medicare and Medicaid programs. We believe that we are following all applicable laws and regulations.
Medicare and Medicaid program revenues, as well as certain Managed Care program revenues, are subject to audit and retroactive adjustment by government representatives or their agents. Settlements with third-party payors for retroactive adjustments due to audits, reviews or investigations are considered variable consideration and are included in the determination of the estimated transaction price for providing patient care. These settlements are estimated based on the terms of the payment agreement with the payor, correspondence from the payor and the Company’s historical settlement activity, including an assessment to ensure that it is probable that a significant reversal in the amount of cumulative revenue recognized will not occur when the uncertainty associated with the retroactive adjustment is subsequently resolved. Estimated settlements are adjusted in future periods as adjustments become known, or as years are settled or are no longer subject to such audits, reviews, and investigations. We believe that any differences between the net revenues recorded, and final determination will not materially affect the consolidated financial statements. We have made provisions of approximately $16,631,000 and $17,595,000 as of December 31, 2022 and 2021, respectively, for various Medicare, Medicaid, and Managed Care claims reviews and current and prior year cost reports.
Note 4 – Other Revenues
Other revenues are outlined in the table below. Revenues from rental income include health care real estate properties owned by us and leased to third party operators. Revenues from management and accounting services include fees provided to manage and provide accounting services to other healthcare operators. Revenues from insurance services include premiums for workers’ compensation and professional liability insurance policies that our wholly owned insurance subsidiaries have written for certain healthcare operators to which we provide management or accounting services. "Other" revenues include miscellaneous health care related earnings (in thousands).
| | | Year Ended December 31, | |
| | | 2022 | | | 2021 | | | 2020 | |
| Rental income | | $ | 23,451 | | | $ | 22,717 | | | $ | 22,768 | |
| Management and accounting service fees | | | 16,160 | | | | 17,139 | | | | 17,147 | |
| Insurance services | | | 4,766 | | | | 5,019 | | | | 5,447 | |
| Other | | | 819 | | | | 525 | | | | 771 | |
| Gain on sale of property and equipment | | | – | | | | – | | | | 2,784 | |
| Total other revenues | | $ | 45,196 | | | $ | 45,400 | | | $ | 48,917 | |
Rental Income
The Company leases real estate assets consisting of skilled nursing facilities and assisted living facilities to third party operators. Additionally, we sublease four Florida skilled nursing facilities included in our lease from National Health Investors (“NHI”) as noted in Note 7 – Long Term Leases. Rental income reflected in the consolidated statements of operations consisted of the following (in thousands):
| | | Year Ended December 31, | |
| | | 2022 | | | 2021 | | | 2020 | |
| Operating lease payments | | $ | 23,039 | | | $ | 22,609 | | | $ | 22,019 | |
| Variable lease payments | | | 412 | | | | 108 | | | | 749 | |
| Total rental income | | $ | 23,451 | | | $ | 22,717 | | | $ | 22,768 | |
The following table sets forth the undiscounted cash flows for future minimum lease payments receivable for leases in effect at December 31, 2022 (in thousands):
| 2023 | | $ | 22,738 | |
| 2024 | | | 22,730 | |
| 2025 | | | 22,730 | |
| 2026 | | | 20,220 | |
| 2027 | | | – | |
| Thereafter | | | – | |
| Total future minimum lease payments | | $ | 88,418 | |
Management Fees from National
We have managed skilled nursing facilities for National since 1988, and we currently manage five facilities. See Note 17 regarding our relationship with National.
During 2022, 2021 and 2020, we recognized approximately $4,332,000, $3,915,000, and $4,729,000, respectively, of management fees and interest on management fees. Unrecognized and unpaid management fees and interest on management fees from National total $18,843,000 and $18,908,000 at December 31, 2022 and 2021, respectively.
The unpaid fees from these five facilities, because collection of substantially all of the contract consideration was not probable when the performance obligation was satisfied, will be recognized as revenues only in the period in which the amounts are received. Under the terms of our management agreement with National, the payment of these fees to us may be subordinated to other expenditures of the five skilled nursing facilities. We continue to manage these facilities so that we may be able to collect our fees in the future and because the incremental savings from discontinuing services to a facility may be small compared to the potential benefit. We may receive payment for the unrecognized management fees in whole or in part in the future only if cash flows from the operating and investing activities of centers or proceeds from the sale of the centers are sufficient to pay the fees. There can be no assurance that such future improved cash flows will occur.
Management Fees and Financial and Accounting Services for Other Healthcare Centers
We provide management services and financial and accounting services to certain healthcare facilities (in addition to the five National centers) operated by third party owners. For the years ended December 31, 2022, 2021 and 2020, we recognized management fees and financial and accounting fees of $11,828,000, $13,224,000, and $12,418,000 from these centers, respectively.
Insurance Services
For workers’ compensation insurance services, the premium revenues reflected in the consolidated statements of operations for the years ended December 31, 2022, 2021 and 2020 were $2,689,000, $2,974,000, and $3,300,000, respectively. Associated losses and expenses are reflected in the consolidated statements of operations as "Salaries, wages and benefits."
For professional liability insurance services, the premium revenues reflected in the consolidated statements of operations for the years ended December 31, 2022, 2021 and 2020 were $2,077,000, $2,045,000, and $2,147,000, respectively. Associated losses and expenses including those for self–insurance are included in the consolidated statements of operations as "Other operating costs and expenses".
Note 5 – Non–Operating Income
Non–operating income includes equity in earnings of unconsolidated investments, dividends and other realized gains and losses on marketable securities, and interest income (in thousands).
| | | Year Ended December 31, | |
| | | 2022 | | | 2021 | | | 2020 | |
| Equity in earnings of unconsolidated investments | | $ | 477 | | | $ | 5,111 | | | $ | 12,342 | |
| Dividends and net realized gains or losses on the sale of securities | | | 5,530 | | | | 7,998 | | | | 8,390 | |
| Interest income | | | 5,134 | | | | 4,665 | | | | 5,795 | |
| Total non-operating income | | $ | 11,141 | | | $ | 17,774 | | | $ | 26,527 | |
Caris HealthCare, L.P. (“Caris”)
On June 11, 2021, the Company acquired the remaining 24.9% equity interest in Caris HealthCare, L.P. (“Caris”). Prior to the June 11, 2021 acquisition date, Caris was our most significant equity method investment with a 75.1% non-controlling ownership interest. From the respective acquisition date, Caris’ financial information is now included in the Company’s consolidated financial statements and is no longer accounted for as an equity method investment.
Note 6 – Business Segments
The Company has two reportable operating segments: (1) inpatient services, which includes the operation of skilled nursing facilities, assisted and independent living facilities, and behavioral health hospitals; and (2) homecare and hospice services. These reportable operating segments are consistent with information used by the Company’s Chief Executive Officer, as chief operating decision maker (“CODM”), to assess performance and allocate resources. The Company also reports an “all other” category that includes revenues from rental income, management and accounting services fees, insurance services, and costs of the corporate office.
The Company’s CODM evaluates performance and allocates capital resources to each segment based on an operating model that is designed to improve the quality of patient care and profitability of the Company while enhancing long-term shareholder value. The CODM does not review assets by segment in his resource allocation and therefore, assets by segment are not disclosed below.
The following tables set forth the Company’s consolidated statements of operations by business segment (in thousands):
| | | Year Ended December 31, 2022 | |
| | | Inpatient Services | | | Homecare and Hospice | | | All Other | | | Total | |
| Revenues: | | | | | | | | | | | | | | | | |
| Net patient revenues | | $ | 900,231 | | | $ | 128,854 | | | $ | – | | | $ | 1,029,085 | |
| Other revenues | | | 136 | | | | – | | | | 45,060 | | | | 45,196 | |
| Government stimulus income | | | 11,457 | | | | – | | | | – | | | | 11,457 | |
| Net operating revenues and grant income | | | 911,824 | | | | 128,854 | | | | 45,060 | | | | 1,085,738 | |
| | | | | | | | | | | | | | | | | |
| Costs and Expenses: | | | | | | | | | | | | | | | | |
| Salaries, wages and benefits | | | 580,707 | | | | 77,688 | | | | 27,774 | | | | 686,169 | |
| Other operating | | | 251,355 | | | | 26,319 | | | | 11,698 | | | | 289,372 | |
| Facility rent | | | 32,956 | | | | 2,327 | | | | 5,694 | | | | 40,977 | |
| Depreciation and amortization | | | 36,522 | | | | 691 | | | | 3,276 | | | | 40,489 | |
| Interest | | | 563 | | | | – | | | | – | | | | 563 | |
| Recovery of assets | | | – | | | | – | | | | (3,728 | ) | | | (3,728 | ) |
| Total costs and expenses | | | 902,103 | | | | 107,025 | | | | 44,714 | | | | 1,053,842 | |
| | | | | | | | | | | | | | | | | |
| Income before non-operating income | | | 9,721 | | | | 21,829 | | | | 346 | | | | 31,896 | |
| Non-operating income | | | – | | | | – | | | | 11,141 | | | | 11,141 | |
| Unrealized losses on marketable equity securities | | | – | | | | – | | | | (15,806 | ) | | | (15,806 | ) |
| | | | | | | | | | | | | | | | | |
| Income (loss) before income taxes | | $ | 9,721 | | | $ | 21,829 | | | $ | (4,319 | ) | | $ | 27,231 | |
| | | Year Ended December 31, 2021 | |
| | | Inpatient Services | | | Homecare and Hospice | | | All Other | | | Total | |
| Revenues: | | | | | | | | | | | | | | | | |
| Net patient revenues | | $ | 868,687 | | | $ | 96,855 | | | $ | – | | | $ | 965,542 | |
| Other revenues | | | 386 | | | | – | | | | 45,014 | | | | 45,400 | |
| Government stimulus income | | | 63,360 | | | | – | | | | – | | | | 63,360 | |
| Net operating revenues and grant income | | | 932,433 | | | | 96,855 | | | | 45,014 | | | | 1,074,302 | |
| | | | | | | | | | | | | | | | | |
| Costs and Expenses: | | | | | | | | | | | | | | | | |
| Salaries, wages and benefits | | | 557,604 | | | | 59,226 | | | | 49,233 | | | | 666,063 | |
| Other operating | | | 238,354 | | | | 16,053 | | | | 12,347 | | | | 266,754 | |
| Facility rent | | | 32,819 | | | | 2,064 | | | | 5,935 | | | | 40,818 | |
| Depreciation and amortization | | | 36,890 | | | | 443 | | | | 3,339 | | | | 40,672 | |
| Interest | | | 845 | | | | – | | | | – | | | | 845 | |
| Impairment of assets | | | 4,497 | | | | – | | | | 3,728 | | | | 8,225 | |
| Total costs and expenses | | | 871,009 | | | | 77,786 | | | | 74,582 | | | | 1,023,377 | |
| | | | | | | | | | | | | | | | | |
| Income (loss) before non-operating income | | | 61,424 | | | | 19,069 | | | | (29,568 | ) | | | 50,925 | |
| Non-operating income | | | – | | | | – | | | | 17,774 | | | | 17,774 | |
| Gain on acquisition of equity method investment | | | – | | | | – | | | | 95,202 | | | | 95,202 | |
| Unrealized losses on marketable equity securities | | | – | | | | – | | | | (13,863 | ) | | | (13,863 | ) |
| | | | | | | | | | | | | | | | | |
| Income before income taxes | | $ | 61,424 | | | $ | 19,069 | | | $ | 69,545 | | | $ | 150,038 | |
61
| | | Year Ended December 31, 2020 | |
| | | Inpatient Services | | | Homecare and Hospice | | | All Other | | | Total | |
| Revenues: | | | | | | | | | | | | | | | | |
| Net patient revenues | | $ | 879,693 | | | $ | 52,102 | | | $ | – | | | $ | 931,795 | |
| Other revenues | | | 3,403 | | | | – | | | | 45,514 | | | | 48,917 | |
| Government stimulus income | | | 47,505 | | | | – | | | | – | | | | 47,505 | |
| Net operating revenues and grant income | | | 930,601 | | | | 52,102 | | | | 45,514 | | | | 1,028,217 | |
| | | | | | | | | | | | | | | | | |
| Costs and Expenses: | | | | | | | | | | | | | | | | |
| Salaries, wages and benefits | | | 546,188 | | | | 37,377 | | | | 37,427 | | | | 620,992 | |
| Other operating | | | 254,230 | | | | 10,416 | | | | 10,513 | | | | 275,159 | |
| Facility rent | | | 33,090 | | | | 1,802 | | | | 5,602 | | | | 40,494 | |
| Depreciation and amortization | | | 38,217 | | | | 377 | | | | 3,424 | | | | 42,018 | |
| Interest | | | 1,374 | | | | – | | | | 25 | | | | 1,399 | |
| Total costs and expenses | | | 873,099 | | | | 49,972 | | | | 56,991 | | | | 980,062 | |
| | | | | | | | | | | | | | | | | |
| Income (loss) before non-operating income | | | 57,502 | | | | 2,130 | | | | (11,477 | ) | | | 48,155 | |
| Non-operating income | | | – | | | | – | | | | 26,527 | | | | 26,527 | |
| Gain on acquisition of equity method investment | | | – | | | | – | | | | 1,707 | | | | 1,707 | |
| Unrealized losses on marketable equity securities | | | – | | | | – | | | | (23,966 | ) | | | (23,966 | ) |
| | | | | | | | | | | | | | | | | |
| Income (loss) before income taxes | | $ | 57,502 | | | $ | 2,130 | | | $ | (7,209 | ) | | $ | 52,423 | |
Note 7 – Long–Term Leases
Operating Leases
At December 31, 2022, we lease from NHI the real property of 28 skilled nursing facilities, five assisted living centers and three independent living centers under one master lease agreement. As part of the lease agreement, we sublease four Florida skilled nursing facilities to a third-party operator. The lease includes base rent plus a percentage rent.
On September 1, 2022, we transferred the operations of seven skilled nursing facilities located in Massachusetts and New Hampshire to a third-party operator. We leased the real property of these seven facilities from NHI under a separate lease agreement. In conjunction with the transfer of the operations to a third party, we terminated our lease agreement for the seven skilled nursing facilities and amended our master lease agreement with NHI. The amendment was accounted for as a lease modification under ASC 842, Leases. The base rent within the amended master lease agreement increased approximately $8,775,000 over the next four and one-third years. The annual base rent in 2023 increased from $30,750,000 to $34,075,000, in 2024 from $30,750,000 to $32,625,000, in 2025 from $30,750,000 to $32,225,000, and in 2026 from $30,750,000 to $31,975,000.
Base rent expense under the NHI lease agreements for 2022, 2021, and 2020 was $33,783,000, $34,200,000, and $34,200,000, respectively. Percentage rent under the master lease agreement is based on a quarterly calculation of revenue increases and is payable on a quarterly basis. Percentage rent expense under the NHI lease agreements for 2022, 2021, and 2020 was $3,887,000, $3,721,000 and $3,617,000, respectively.
We have a right of first refusal with NHI to purchase any of the properties should NHI receive an offer from an unrelated party during the term of the lease or up to 180 days after termination of the related lease.
Finance Leases
Effective June 1, 2014, NHC began leasing and operating three senior healthcare facilities in the state of Missouri under three separate lease agreements. Two of the healthcare facilities are skilled nursing facilities that also include assisted living facilities and the third healthcare facility is a memory care facility. Each of the leases is a ten-year lease with two five–year renewal options. Under the terms of the leases, base rent totals $5,200,000 annually with rent thereafter escalating by 4% of the increase in facility revenue over the 2014 base year.
Fixed assets recorded under the finance leases, which are included in property and equipment in the consolidated balance sheets, are as follows (in thousands):
| | | December 31, | |
| | | 2022 | | | 2021 | |
| Buildings and personal property | | $ | 39,011 | | | $ | 39,014 | |
| Accumulated amortization | | | (34,482 | ) | | | (30,604 | ) |
| | | $ | 4,529 | | | $ | 8,410 | |
Lease Classification
The Company recorded the following on the consolidated balance sheets (in thousands):
| | | | | December 31, | |
| Right-of-Use Assets | | Balance Sheet Classification | | 2022 | | | 2021 | |
| Finance lease assets | | Net property and equipment | | $ | 4,529 | | | $ | 8,410 | |
| Operating lease right-of use assets | | Operating lease right-of-use assets | | | 120,521 | | | | 156,116 | |
| Total | | $ | 125,050 | | | $ | 164,526 | |
| | | | | December 31, | |
| Lease Liabilities | | Balance Sheet Classification | | 2022 | | | 2021 | |
| Current: | | | | | | | | | | |
| Finance lease liabilities | | Finance lease obligations, current portion | | $ | 4,985 | | | $ | 4,695 | |
| Operating lease liabilities | | Operating lease liabilities, current portion | | | 29,075 | | | | 27,574 | |
| Noncurrent: | | | | | | | | | | |
| Finance lease liabilities | | Finance lease obligations, less current portion | | | 860 | | | | 5,845 | |
| Operating lease liabilities | | Operating lease liabilities, less current portion | | | 91,016 | | | | 128,542 | |
| Total | | $ | 125,936 | | | $ | 166,656 | |
Weighted-average remaining lease terms and discount rates were as follows:
| | | December 31, | |
| | | 2022 | | | 2021 | |
| Weighted-average remaining lease terms (in years) | | | | | | | | |
| Finance | | | 1.2 | | | | 2.2 | |
| Operating | | | 4.0 | | | | 5.2 | |
| | | | | | | | | |
| Weighted-average discount rate | | | | | | | | |
| Finance | | | 6.0% | | | | 6.0% | |
| Operating | | | 6.6% | | | | 6.0% | |
Lease Costs
Lease costs recorded in the consolidated statement of operations are as follows (in thousands):
| | | December 31, | |
| | | 2022 | | | 2021 | | | 2020 | |
| Finance lease costs: | | | | | | | | | | | | |
| Depreciation of leased assets | | $ | 3,878 | | | $ | 3,905 | | | $ | 3,906 | |
| Interest of lease liabilities | | | 534 | | | | 807 | | | | 1,064 | |
| Total finance lease costs | | | 4,412 | | | | 4,712 | | | | 4,970 | |
| | | | | | | | | | | | | |
| Operating lease costs: | | | | | | | | | | | | |
| Operating lease costs | | | 36,051 | | | | 36,079 | | | | 35,656 | |
| Variable lease costs | | | 3,887 | | | | 3,721 | | | | 3,617 | |
| Short-term lease costs | | | 1,039 | | | | 1,018 | | | | 1,221 | |
| Total operating lease costs | | | 40,977 | | | | 40,818 | | | | 40,494 | |
| | | | | | | | | | | | | |
| Total lease costs | | $ | 45,389 | | | $ | 45,530 | | | $ | 45,464 | |
63
Minimum Lease Payments
The following table summarizes the maturity of our finance and operating lease liabilities as of December 31, 2022 (in thousands):
| | | Finance Leases | | | Operating Leases | |
| 2023 | | $ | 5,200 | | | $ | 35,973 | |
| 2024 | | | 867 | | | | 34,013 | |
| 2025 | | | – | | | | 33,224 | |
| 2026 | | | – | | | | 32,589 | |
| 2027 | | | – | | | | 208 | |
| Thereafter | | | – | | | | – | |
| Total minimum lease payments | | $ | 6,067 | | | $ | 136,007 | |
| Less: amounts representing interest | | | (222 | ) | | | (15,916 | ) |
| Present value of future minimum lease payments | | | 5,845 | | | | 120,091 | |
| Less: current portion | | | (4,985 | ) | | | (29,075 | ) |
| Noncurrent lease liabilities | | $ | 860 | | | $ | 91,016 | |
Other
Supplemental cash flow data were as follows (in thousands):
| | | December 31, | |
| | | 2022 | | | 2021 | | | 2020 | |
| Cash paid for amounts included in the measurement of lease liabilities: | | | | | | | | | | | | |
| Operating cash flows for operating leases | | $ | 36,051 | | | $ | 36,079 | | | $ | 35,656 | |
| Operating cash flows for finance leases | | | 534 | | | | 807 | | | | 1,064 | |
| Financing cash flows for finance leases | | | 4,695 | | | | 4,423 | | | | 4,166 | |
Note 8 – Earning Per Share
The following table summarizes the earnings and the weighted average number of common shares used in the calculation of basic and diluted earnings per share (in thousands, except share and per share amounts):
| | | Year Ended December 31, | |
| | | 2022 | | | 2021 | | | 2020 | |
| Basic: | | | | | | | | | | | | |
| Weighted average common shares outstanding | | | 15,410,222 | | | | 15,347,129 | | | | 15,306,174 | |
| Net income attributable to common stockholders of National Healthcare Corporation | | $ | 22,445 | | | $ | 138,590 | | | $ | 41,871 | |
| | | | | | | | | | | | | |
| Earnings per common share, basic | | $ | 1.46 | | | $ | 9.03 | | | $ | 2.74 | |
| | | | | | | | | | | | | |
| Diluted: | | | | | | | | | | | | |
| Weighted average common shares outstanding | | | 15,410,222 | | | | 15,347,129 | | | | 15,306,174 | |
| Dilutive effect of stock options | | | 36,989 | | | | 69,587 | | | | 63,349 | |
| Assumed average common shares outstanding | | | 15,447,211 | | | | 15,416,716 | | | | 15,369,523 | |
| | | | | | | | | | | | | |
| Net income attributable to common stockholders of National Healthcare Corporation | | $ | 22,445 | | | $ | 138,590 | | | $ | 41,871 | |
| | | | | | | | | | | | | |
| Earnings per common share, diluted | | $ | 1.45 | | | $ | 8.99 | | | $ | 2.72 | |
In the above table, options to purchase 375,638, 291,946, and 713,956 shares of our common stock have been excluded for the years ended December 31, 2022, 2021, and 2020, respectively, due to their anti-dilutive impact.
Note 9 – Investments in Marketable Securities
Marketable securities consist of the following (in thousands):
| | | December 31, 2022 | | | December 31, 2021 | |
| | | Amortized Cost | | | Fair Value | | | Amortized Cost | | | Fair Value | |
| Investments available for sale: | | | | | | | | | | | | | | | | |
| Marketable equity securities | | $ | 30,176 | | | $ | 100,786 | | | $ | 30,176 | | | $ | 113,108 | |
| Corporate debt securities | | | 14,317 | | | | 13,885 | | | | 19,038 | | | | 18,843 | |
| Asset-backed securities | | | 500 | | | | 494 | | | | 1,481 | | | | 1,469 | |
| U.S. Treasury securities | | | 9,009 | | | | 8,757 | | | | 15,082 | | | | 14,998 | |
| Restricted investments available for sale: | | | | | | | | | | | | | |
| Marketable equity securities | | | 24,326 | | | | 22,358 | | | | 25,442 | | | | 26,958 | |
| Corporate debt securities | | | 54,412 | | | | 51,009 | | | | 60,816 | | | | 62,936 | |
| Asset–backed securities | | | 24,605 | | | | 22,437 | | | | 32,918 | | | | 33,301 | |
| U.S. Treasury securities | | | 45,989 | | | | 41,294 | | | | 33,052 | | | | 32,630 | |
| State and municipal securities | | | 4,877 | | | | 4,771 | | | | 7,700 | | | | 7,923 | |
| | | $ | 208,211 | | | | 265,791 | | | $ | 225,705 | | | $ | 312,166 | |
Included in the marketable equity securities available for sale are the following (in thousands, except share amounts):
| | | December 31, 2022 | | | December 31, 2021 | |
| | | Shares | | | Cost | | | Fair Value | | | Shares | | | Cost | | | Fair Value | |
| NHI Common Stock | | | 1,630,642 | | | $ | 24,734 | | | $ | 85,152 | | | | 1,630,642 | | | $ | 24,734 | | | $ | 93,713 | |
The amortized cost and estimated fair value of debt securities classified as available for sale, by contractual maturity, are as follows (in thousands):
| | | December 31, 2022 | | | December 31, 2021 | |
| | | Cost | | | Fair Value | | | Cost | | | Fair Value | |
| Maturities: | | | | | | | | | | | | | | | | |
| Within 1 year | | $ | 33,662 | | | $ | 33,037 | | | $ | 32,718 | | | $ | 32,843 | |
| 1 to 5 years | | | 81,500 | | | | 76,394 | | | | 95,293 | | | | 96,937 | |
| 6 to 10 years | | | 38,547 | | | | 33,216 | | | | 41,580 | | | | 41,835 | |
| Over 10 years | | | – | | | | – | | | | 496 | | | | 485 | |
| | | $ | 153,709 | | | $ | 142,647 | | | $ | 170,087 | | | $ | 172,100 | |
Gross unrealized gains related to marketable equity securities are $71,869,000 and $85,394,000 as of December 31, 2022 and 2021, respectively. Gross unrealized losses related to marketable equity securities are $3,227,000 and $946,000 as of December 31, 2022 and 2021, respectively. For the years ended December 31, 2022, 2021, and 2020 the Company recognized net unrealized losses of $15,806,000, 13,863,000, and $23,966,000, respectively, in the consolidated statements of operations.
Gross unrealized gains related to available for sale marketable debt securities are $9,000 and $3,189,000 as of December 31, 2022 and 2021, respectively. Gross unrealized losses related to available for sale marketable debt securities are $11,071,000 and $1,176,000 as of December 31, 2022 and 2021, respectively.
The Company’s unrealized losses in our available for sale marketable debt securities were determined to be non-credit related. The Company has not recognized any credit related impairments for the years ended December 31, 2022 and 2021.
For the marketable debt securities in gross unrealized loss positions, (a) it is more likely than not that the Company will not be required to sell the investment securities before recovery of the unrealized losses, and (b) the Company expects that the contractual principal and interest will be received on the investment securities.
Proceeds from the sale of available for sale marketable securities during the years ended December 31, 2022, 2021, and 2020 were $49,961,000, $101,920,000, and $40,994,000, respectively. Net investment losses of $1,326,000 and net investment gains of $1,042,000 and $195,000 were realized on these sales during the years ended December 31, 2022, 2021, and 2020, respectively.
Note 10 – Fair Value Measurements
The accounting standard for fair value measurements provides a framework for measuring fair value and requires expanded disclosures regarding fair value measurements. Fair value is defined as the price that would be received for an asset or the exit price that would be paid to transfer a liability in the principal or most advantageous market in an orderly transaction between market participants on the measurement date. This accounting standard establishes a fair value hierarchy, which requires an entity to maximize the use of observable inputs, where available. The following summarizes the three levels of inputs that may be used to measure fair value:
Level 1 – The valuation is based on quoted prices in active markets for identical instruments.
Level 2 – The valuation is based on observable inputs such as quoted prices for similar instruments in active markets, quoted prices for identical or similar instruments in markets that are not active, and model–based valuation techniques for which all significant assumptions are observable in the market.
Level 3 – The valuation is based on unobservable inputs that are supported by minimal or no market activity and that are significant to the fair value of the instrument. Level 3 valuations are typically performed using pricing models, discounted cash flow methodologies, or similar techniques that incorporate management’s own estimates of assumptions that market participants would use in pricing the instrument, or valuations that require significant management judgment or estimation.
A financial instrument’s level within the fair value hierarchy is based on the lowest level of input that is significant to the fair value measurement.
The Company's non-financial assets, which includes goodwill, intangible assets, property and equipment and right-of-use assets, are not required to be measured at fair value on a recurring basis. However, on a periodic basis, or whenever events or changes in circumstances indicate that their carrying value may not be recoverable, the Company assesses its long-lived assets for impairment. When impairment has occurred, such long-lived assets are written down to fair value.
Valuation of Marketable Securities
The Company determines fair value for marketable securities with Level 1 inputs through quoted market prices. The Company determines fair value for marketable securities with Level 2 inputs through broker or dealer quotations or alternative pricing sources with reasonable levels of price transparency. Our Level 2 marketable securities have been initially valued at the transaction price and subsequently valued, at the end of each month, typically utilizing third party pricing services or other market observable data. The pricing services utilize industry standard valuation models, including both income and market-based approaches and observable market inputs to determine value. These observable market inputs include reportable trades, benchmark yields, credit spreads, broker/dealer quotes, bids, offers, and other industry and economic events.
We validated the prices provided by our broker by reviewing their pricing methods, obtaining market values from other pricing sources, analyzing pricing data in certain instances and confirming that the relevant markets are active. After completing our validation procedures, we did not adjust or override any fair value measurements provided by our broker as of December 31, 2022 or 2021.
Other
The carrying amounts of cash and cash equivalents, restricted cash and cash equivalents, accounts receivable, and accounts payable approximate fair value due to their short–term nature. The estimated fair value of notes receivable approximates the carrying value based principally on their underlying interest rates and terms, maturities, collateral and credit status of the receivables. At December 31, 2022 and 2021, there were no material differences between the carrying amounts and fair values of NHC’s financial instruments.
66
The following table summarizes fair value measurements by level at December 31, 2022 and December 31, 2021 for assets and liabilities measured at fair value on a recurring basis (in thousands):
| |
|
Fair Value Measurements Using |
|
| December 31, 2022 |
|
Fair Value |
|
|
Quoted Prices in Active Markets For Identical Assets (Level 1) |
|
|
Significant Other Observable Inputs (Level 2) |
|
|
Significant Unobservable Inputs (Level 3) |
|
| Cash and cash equivalents |
|
$ |
58,667 |
|
|
$ |
58,667 |
|
|
$ |
– |
|
|
$ |
– |
|
| Restricted cash and cash equivalents |
|
|
16,198 |
|
|
|
16,198 |
|
|
|
– |
|
|
|
– |
|
| Marketable equity securities |
|
|
123,144 |
|
|
|
123,144 |
|
|
|
– |
|
|
|
– |
|
| Corporate debt securities |
|
|
64,894 |
|
|
|
48,525 |
|
|
|
16,369 |
|
|
|
– |
|
| Asset–backed securities |
|
|
22,931 |
|
|
|
– |
|
|
|
22,931 |
|
|
|
– |
|
| U.S. Treasury securities |
|
|
50,051 |
|
|
|
50,051 |
|
|
|
– |
|
|
|
– |
|
| State and municipal securities |
|
|
4,771 |
|
|
|
1,337 |
|
|
|
3,434 |
|
|
|
– |
|
| Total financial assets |
|
$ |
340,656 |
|
|
$ |
297,922 |
|
|
$ |
42,734 |
|
|
$ |
– |
|
| |
|
Fair Value Measurements Using |
|
| December 31, 2021 |
|
Fair Value |
|
|
Quoted Prices in Active Markets For Identical Assets (Level 1) |
|
|
Significant Other Observable Inputs (Level 2) |
|
|
Significant Unobservable Inputs (Level 3) |
|
| Cash and cash equivalents |
|
$ |
107,607 |
|
|
$ |
107,607 |
|
|
$ |
– |
|
|
$ |
– |
|
| Restricted cash and cash equivalents |
|
|
12,136 |
|
|
|
12,136 |
|
|
|
– |
|
|
|
– |
|
| Marketable equity securities |
|
|
140,066 |
|
|
|
140,066 |
|
|
|
– |
|
|
|
– |
|
| Corporate debt securities |
|
|
81,779 |
|
|
|
50,005 |
|
|
|
31,774 |
|
|
|
– |
|
| Asset–backed securities |
|
|
34,770 |
|
|
|
– |
|
|
|
34,770 |
|
|
|
– |
|
| U.S. Treasury securities |
|
|
47,628 |
|
|
|
47,628 |
|
|
|
– |
|
|
|
– |
|
| State and municipal securities |
|
|
7,923 |
|
|
|
– |
|
|
|
7,923 |
|
|
|
– |
|
| Total financial assets |
|
$ |
431,909 |
|
|
$ |
357,442 |
|
|
$ |
74,467 |
|
|
$ |
– |
|
Note 11 – Property and Equipment
Property and equipment, at cost, consists of the following (in thousands):
| | | December 31, | |
| | | 2022 | | | 2021 | |
| Land | | $ | 67,165 | | | $ | 66,267 | |
| Leasehold improvements | | | 125,142 | | | | 122,391 | |
| Buildings and improvements | | | 688,433 | | | | 654,656 | |
| Furniture and equipment | | | 187,743 | | | | 185,320 | |
| Construction in progress | | | 12,736 | | | | 35,703 | |
| Property and equipment, at cost | | | 1,081,219 | | | | 1,064,337 | |
| Less: Accumulated depreciation | | | (574,687 | ) | | | (543,341 | ) |
| Net property and equipment | | $ | 506,532 | | | $ | 520,996 | |
Note 12 – Goodwill and Other Intangible Assets
As of December 31, 2022, we evaluated potential triggering events that might be indicators that our goodwill and indefinite lived intangibles were impaired. The Company performs its goodwill impairment analysis for each reporting unit that constitutes a component for which (1) discrete financial information is available and (2) segment management regularly reviews the operating results of that component, in accordance with the provisions of ASC Topic 350, Intangibles - Goodwill and Other. No goodwill or intangible asset impairments were recorded during the years ended December 31, 2022, 2021, and 2020.
The following table represents activity in goodwill by segment as of and for the year ended December 31, 2022 (in thousands):
| | | Year Ended December 31, 2022 | |
| | | Inpatient Services | | | Homecare | | | All Other | | | Total | |
| January 1, 2020 | | $ | 3,395 | | | $ | 17,600 | | | $ | – | | | $ | 20,995 | |
| Additions | | | 346 | | | | – | | | | – | | | | 346 | |
| December 31, 2020 | | | 3,741 | | | | 17,600 | | | | – | | | | 21,341 | |
| Additions | | | – | | | | 146,954 | | | | – | | | | 146,954 | |
| December 31, 2021 | | | 3,741 | | | | 164,554 | | | | – | | | | 168,295 | |
| Additions | | | – | | | | – | | | | – | | | | – | |
| December 31, 2022 | | $ | 3,741 | | | $ | 164,554 | | | $ | – | | | $ | 168,295 | |
As part of the Caris acquisition in June 2021, we also recorded indefinite-lived intangible assets that consisted of the trade name ($4,340,000) and certificates of need and licenses ($2,698,000).
Note 13 – Income Taxes
The provision for income taxes is comprised of the following components (in thousands):
| | | Year Ended December 31, | |
| | | 2022 | | | 2021 | | | 2020 | |
| Current tax provision | | | | | | | | | | | | |
| Federal | | $ | 717 | | | $ | 15,072 | | | $ | 19,054 | |
| State | | | 251 | | | | 1,164 | | | | 2,337 | |
| Total current tax provision | | | 968 | | | | 16,236 | | | | 21,391 | |
| Deferred tax provision | | | | | | | | | | | | |
| Federal | | | 4,595 | | | | (3,866 | ) | | | (8,349 | ) |
| State | | | 1,691 | | | | (1,419 | ) | | | (2,609 | ) |
| Total deferred tax provision | | | 6,286 | | | | (5,285 | ) | | | (10,958 | ) |
| Income tax provision | | $ | 7,254 | | | $ | 10,951 | | | $ | 10,433 | |
68
The deferred tax assets and liabilities, consisting of temporary differences tax effected at the respective income tax rates, are as follows (in thousands):
| | | December 31, | |
| | | 2022 | | | 2021 | |
| Deferred tax assets: | | | | | | | | |
| Accrued risk reserves | | $ | 2,209 | | | $ | 1,803 | |
| Accrued expenses | | | 6,441 | | | | 9,663 | |
| Financial reporting depreciation in excess of tax depreciation | | | 5,505 | | | | 5,610 | |
| Stock based compensation | | | 742 | | | | 527 | |
| Deferred revenue | | | 3,393 | | | | 8,019 | |
| Operating lease liabilities | | | 30,558 | | | | 39,629 | |
| Other | | | 1,711 | | | | 1,991 | |
| Total gross deferred tax assets | | | 50,559 | | | | 67,242 | |
| Less: valuation allowance | | | (978 | ) | | | – | |
| Deferred tax assets less valuation allowance | | $ | 49,581 | | | $ | 67,242 | |
| | | | | | | | | |
| Deferred tax liabilities: | | | | | | | | |
| Unrealized gains on marketable securities | | $ | (15,396 | ) | | $ | (22,401 | ) |
| Deferred gain on sale of assets, net | | | (2,045 | ) | | | (2,040 | ) |
| Book basis in excess of tax basis of intangible assets | | | (3,063 | ) | | | (2,708 | ) |
| Book basis in excess of tax basis of securities | | | (3,164 | ) | | | (2,822 | ) |
| Long–term investments | | | (6,155 | ) | | | (4,494 | ) |
| Operating lease assets | | | (30,667 | ) | | | (39,629 | ) |
| Total deferred tax liabilities | | $ | (60,490 | ) | | $ | (74,094 | ) |
| | | | | | | | | |
| Net deferred tax liability | | $ | (10,909 | ) | | $ | (6,852 | ) |
A reconciliation of income tax expense and the amount computed by applying the statutory federal income tax rate to income before income taxes is as follows (in thousands):
| | | Year Ended December 31, | |
| | | 2022 | | | 2021 | | | 2020 | |
| Tax provision at federal statutory rate | | $ | 5,719 | | | $ | 31,508 | | | $ | 11,009 | |
| | | | | | | | | | | | | |
| Increase (decrease) in income taxes resulting from: | | | | | | | | | | | | |
| State, net of federal benefit | | | 1,034 | | | | 1,113 | | | | 1,631 | |
| Nontaxable revaluation gain | | | – | | | | (19,758 | ) | | | – | |
| Unrecognized tax benefits | | | 730 | | | | (158 | ) | | | 166 | |
| Expiration of statute of limitations | | | (1,032 | ) | | | (1,901 | ) | | | (2,366 | ) |
| Tax (expense) benefit of minority interest | | | 518 | | | | (104 | ) | | | (30 | ) |
| Other | | | 285 | | | | 251 | | | | 23 | |
| Total increases (decreases) | | | 1,535 | | | | (20,557 | ) | | | (576 | ) |
| Effective income tax expense | | $ | 7,254 | | | $ | 10,951 | | | $ | 10,433 | |
Our deferred tax assets have been evaluated for realization based on historical taxable income, tax planning strategies, the expected timing of reversals of existing temporary differences and future taxable income anticipated. Our deferred tax assets, with the exception of certain state tax net operating losses and certain deferred tax assets associated with unrealized losses on marketable securities, are more likely than not to be realized in full due to the existence of sufficient taxable income of the appropriate character under the tax law. As such, the only valuation allowance relates to state net operating losses and unrealized losses on marketable securities.
Uncertain tax positions may arise where tax laws may allow for alternative interpretations or where the timing of recognition of income is subject to judgment. Under ASC Topic 740, tax positions are evaluated for recognition using a more–likely–than–not threshold, and those tax positions requiring recognition are measured at the largest amount of tax benefit that is greater than 50 percent likely of being realized upon ultimate settlement with a taxing authority that has full knowledge of all relevant information.
In accordance with current guidance, the Company has established a liability for unrecognized tax benefits, which are differences between a tax position taken or expected to be taken in a tax return and the benefit recognized and measured. Generally, a liability is created for an unrecognized tax benefit because it represents a company’s potential future obligation to a taxing authority for a tax position that was not recognized per above. We believe that our liabilities reflect the anticipated outcome of known uncertain tax positions in conformity with ASC Topic 740 Income Taxes. Our liabilities for unrecognized tax benefits are presented in the consolidated balance sheets within other noncurrent liabilities.
A reconciliation of the beginning and ending amount of unrecognized tax benefits is as follows (in thousands):
| | | Deferred Tax Asset | | | Liability For Unrecognized Tax Benefits | | | Liability For Interest and Penalties | | | Liability Total | |
| Balance, January 1, 2020 | | $ | 7,413 | | | $ | 12,749 | | | $ | 3,309 | | | $ | 16,058 | |
| Additions based on tax positions related to the current year | | | 1,229 | | | | 1,229 | | | | – | | | | 1,229 | |
| Additions (reductions) for tax positions of prior years | | | (2,432 | ) | | | (2,273 | ) | | | 403 | | | | (1,870 | ) |
| Reductions for statute of limitation expirations | | | (544 | ) | | | (1,812 | ) | | | (1,098 | ) | | | (2,910 | ) |
| Balance, December 31, 2020 | | | 5,666 | | | | 9,893 | | | | 2,614 | | | | 12,507 | |
| Additions based on tax positions related to the current year | | | 665 | | | | 665 | | | | – | | | | 665 | |
| Additions (reductions) for tax positions of prior years | | | (441 | ) | | | (187 | ) | | | 543 | | | | 356 | |
| Reductions for statute of limitation expirations | | | (435 | ) | | | (1,469 | ) | | | (867 | ) | | | (2,336 | ) |
| Balance, December 31, 2021 | | | 5,455 | | | | 8,902 | | | | 2,290 | | | | 11,192 | |
| Additions based on tax positions related to the current year | | | 636 | | | | 636 | | | | – | | | | 636 | |
| Additions (reductions) for tax positions of prior years | | | (1,097 | ) | | | (273 | ) | | | 900 | | | | 627 | |
| Reductions for statute of limitation expirations | | | (240 | ) | | | (760 | ) | | | (512 | ) | | | (1,272 | ) |
| Balance, December 31, 2022 | | $ | 4,754 | | | $ | 8,505 | | | $ | 2,678 | | | $ | 11,183 | |
Unrecognized tax benefits of $4,109,000, net of federal benefit at December 31, 2022, attributable to permanent differences, would favorably impact our effective tax rate if recognized. We do not expect significant increases or decreases in unrecognized tax benefits for the 2023 year, except for the effect of decreases related to the lapse of statute of limitations estimated at $1,656,000.
Interest and penalties expense related to U.S. federal and state income tax returns are included within income tax expense. The Company is no longer subject to U.S. federal and state examinations by tax authorities for years before 2019 (with few state exceptions).
Note 14 – Stock Repurchases
During 2022, the Company purchased 148,547 shares of its common stock for a total cost of $9,903,000. The shares were funded from cash on hand and were cancelled and returned to the status of authorized but unissued.
Note 15 – Stock–Based Compensation
NHC recognizes stock–based compensation for all stock options and restricted stock granted over the requisite service period using the fair value for these grants as estimated at the date of grant either using the Black–Scholes pricing model for stock options or the quoted market price for restricted stock.
The Compensation Committee of the Board of Directors ("the Committee") has the authority to select the participants to be granted options; to designate whether the option granted is an incentive stock option ("ISO"), a non–qualified option, or a stock appreciation right; to establish the number of shares of common stock that may be issued upon exercise of the option; to establish the vesting provision for any award; and to establish the term any award may be outstanding. The exercise price of any ISO’s granted will not be less than 100% of the fair market value of the shares of common stock on the date granted and the term of an ISO may not be any more than ten years. The exercise price of any non–qualified options granted will not be less than 100% of the fair market value of the shares of common stock on the date granted unless so determined by the Committee.
In May 2020, our stockholders approved the 2020 Omnibus Equity Incentive Plan (the “2020 Equity Incentive Plan”) pursuant to which 2,500,000 shares of our common stock were available to grant for restricted stock, stock appreciation rights, stock options, and employee stock purchase plans. At December 31, 2022, 2,042,701 shares were available for future grants under the 2020 Equity Incentive Plan.
Additionally, we have an employee stock purchase plan that allows employees to purchase our shares of stock through payroll deductions. The plan allows employees to terminate participation at any time.
Compensation expense is recognized only for the awards that ultimately vest. The Company accounts for forfeitures when they occur. Stock–based compensation totaled $2,612,000, $2,620,000, and $2,453,000, for the years ended December 31, 2022, 2021, and 2020, respectively. Stock–based compensation is included in salaries, wages and benefits in the consolidated statements of operations. The total intrinsic value of shares exercised (and tax deductions taken) was $583,000, $2,844,000, and $677,000 for the years ended December 31, 2022, 2021 and 2020, respectively.
At December 31, 2022, the Company had $3,182,000 of unrecognized compensation cost related to unvested stock-based compensation awards. This unrecognized compensation cost will be amortized over an approximate two and a half year period.
Stock Options
The Company is required to estimate the fair value of stock–based awards on the date of grant. The fair value of each option award is estimated using the Black–Scholes option valuation model with the weighted average assumptions indicated in the following table. Each grant is valued as a single award with an expected term based upon expected employment and termination behavior. Compensation cost is recognized over the requisite service period in a manner consistent with the option vesting provisions. The straight–line attribution method requires that compensation expense is recognized at least equal to the portion of the grant–date fair value that is vested at that date. The expected volatility is derived using weekly historical data for periods immediately preceding the date of grant. The risk–free interest rate is the approximate yield on the United States Treasury Strips having a life equal to the expected option life on the date of grant. The expected life is an estimate of the number of years an option will be held before it is exercised. The following table summarizes the assumptions used to value the options granted in the periods shown.
| | | Year Ended December 31, | |
| | | 2022 | | | 2021 | | | 2020 | |
| Risk–free interest rate | | | 1.83% | | | | 0.21% | | | | 0.87% | |
| Expected volatility | | | 31.4% | | | | 34.9% | | | | 20.1% | |
| Expected life, in years | | | 2.9 | | | | 2.2 | | | | 2.2 | |
| Expected dividend yield | | | 3.57% | | | | 3.00% | | | | 2.91% | |
The following table summarizes option activity:
| | | Number of Shares | | | Weighted Average Exercise Price | | | Aggregate Intrinsic Value | |
| Options outstanding at January 1, 2020 | | | 809,529 | | | $ | 71.24 | | | | − | |
| Options granted | | | 104,057 | | | | 73.98 | | | | − | |
| Options exercised | | | (43,630 | ) | | | 63.37 | | | | − | |
| Options cancelled | | | (3,000 | ) | | | 72.94 | | | | − | |
| Options outstanding at December 31, 2020 | | | 866,956 | | | | 72.11 | | | | − | |
| Options granted | | | 55,706 | | | | 70.80 | | | | − | |
| Options exercised | | | (541,736 | | | | 71.39 | | | | − | |
| Options cancelled | | | (6,000 | ) | | | 72.94 | | | | − | |
| Options outstanding at December 31, 2021 | | | 374,926 | | | | 72.95 | | | | − | |
| Options granted | | | 302,266 | | | | 64.72 | | | | − | |
| Options exercised | | | (32,597 | ) | | | 64.49 | | | | − | |
| Options cancelled | | | (199,451 | ) | | | 75.98 | | | | − | |
| Options outstanding at December 31, 2022 | | | 445,144 | | | | 66.62 | | | | − | |
| | | | | | | | | | | | | |
| Options exercisable at December 31, 2022 | | | 157,901 | | | $ | 69.78 | | | $ | − | |
71
| Options Outstanding December 31, 2022 | | | Exercise Prices | | | Weighted
Average Exercise
Price | | | Weighted Average Remaining
Contractual Life in
Years | |
| | 356,749 | | | $61.90 | – | $69.19 | | | $ | 64.61 | | | | 3.7 | |
| | 88,395 | | | $71.64 | – | $77.92 | | | | 74.72 | | | | 2.4 | |
| | 445,144 | | | | | | | | $ | 66.62 | | | | 3.4 | |
Note 16 – Contingencies and Guarantees
Accrued Risk Reserves
We are self–insured for risks related to health insurance and have wholly–owned limited purpose insurance companies that insure risks related to workers’ compensation and general and professional liability insurance claims both for our owned and leased entities and certain of the entities to which we provide management or accounting services. The liability we have recognized for reported claims and estimates for incurred but unreported claims totals $102,469,000 and $98,048,000 at December 31, 2022 and 2021, respectively. The liability is included in accrued risk reserves in the consolidated balance sheets and is subject to adjustment for actual claims incurred. It is possible that these claims plus unasserted claims could exceed our insurance coverages and our reserves, which could have a material adverse effect on our consolidated financial position, results of operations and cash flows.
As a result of the terms of our insurance policies and our use of wholly owned limited purpose insurance companies, we have retained significant insurance risk with respect to workers’ compensation and general and professional liability. We consider the professional services of independent actuaries to assist us in estimating our exposures for claims obligations (for both asserted and unasserted claims) related to deductibles and exposures in excess of coverage limits, and we maintain reserves for these obligations. Such estimates are based on many variables including historical and statistical information and other factors.
Workers’ Compensation
For workers’ compensation, we utilize a wholly owned Tennessee domiciled property/casualty insurance company to write coverage for NHC affiliates and for third–party customers. Policies are written for a duration of twelve months and cover only risks related to workers’ compensation losses. All customers are companies which operate in the long–term care industry. Business is written on a direct basis.
General and Professional Liability Insurance and Lawsuits
The senior care industry has experienced significant increases in both the number of personal injury/wrongful death claims and in the severity of awards based upon alleged negligence by skilled nursing facilities and their employees in providing care to residents. The Company has been, and continues to be, subject to claims and legal actions that arise in the ordinary course of business, including potential claims related to patient care and treatment. The defense of these lawsuits may result in significant legal costs, regardless of the outcome, and can result in large settlement amounts or damage awards.
Insurance coverage for all years includes primary policies and excess policies. The primary coverage is in the amount of a per incident claim and a per location claim with an annual primary policy aggregate limit that is adjusted on an annual basis. Additional insurance is purchased through third party providers that serve to supplement the coverage provided through our wholly owned captive insurance company.
There is certain additional litigation incidental to our business, none of which, based upon information available to date, would be material to our financial position, results of operations, or cash flows. In addition, the long–term care industry is continuously subject to scrutiny by governmental regulators, which could result in litigation or claims related to regulatory compliance matters.
Qui Tam Litigation
United States of America, ex rel. Jennifer Cook and Sally Gaither v. Integrated Behavioral Health, Inc., NHC HealthCare/Moulton, LLC, et al., Case No. 2:20-CV-00877-AMM (N.D. Ala.) This is a qui tam case originally filed under seal on June 22, 2020. The United States declined intervention on March 1, 2021. Thereafter, the Plaintiff filed an amended Complaint against Dr. Sanja Malhotra, Integrated Behavioral Health, Inc. and other entities that Dr. Malhotra is alleged to own or in which he has a financial interest. The Complaint also named multiple skilled nursing facilities as Defendants, including NHC Healthcare/Moulton, LLC, an affiliate of National HealthCare Corporation. The Complaint alleges that nurse practitioners affiliated with Dr. Malhotra provided free services to the facilities in exchange for referrals to entities owned by or in which Dr. Malhotra had a financial interest in violation of the False Claims Act and Anti-Kickback Statute. NHC Healthcare/Moulton, LLC denies the allegations and is vigorously defending the claim. A motion to dismiss was filed on November 4, 2021. On January 28, 2022, the district court stayed this matter and administratively terminated the motion to dismiss pending the U.S. Supreme Court's review of a petition for certiorari filed in an unrelated matter but involving one of the legal arguments raised in the motion to dismiss. The U.S. Supreme Court recently denied the petition for certiorari in the unrelated matter. As a result, NHC Healthcare/Moulton, LLC’s motion to dismiss has been renewed and is now pending before the district court.
Governmental Regulations
Laws and regulations governing the Medicare, Medicaid and other federal healthcare programs are complex and subject to interpretation. Management believes that it is following all applicable laws and regulations in all material respects. However, compliance with such laws and regulations can be subject to future government review and interpretation as well as significant regulatory action including fines, penalties, and exclusions from the Medicare, Medicaid and other federal healthcare programs. There have been several enacted federal and state relief measures as a result of COVID-19 which have provided substantial support to us during this pandemic.
Debt Guarantees
At December 31, 2022, no agreement to guarantee the debt of other parties exists.
Note 17 – Relationship with National Health Corporation
National Health Corporation ("National"), which is wholly owned by the National Health Corporation Leveraged Employee Stock Ownership Plan ("ESOP"), was formed in 1986 and is our administrative services affiliate and contractor. As discussed below, all of the personnel conducting our business, including our executive management team, are employees of National and may have ownership interests in National only through their participation as employees in the ESOP.
Management Contracts
We currently manage five skilled nursing facilities for National under a management contract. The management contract has been extended until January 1, 2028. See Note 4 for additional information regarding management services fees recognized from National.
Financing Activities
In conjunction with our management contract, we have entered into a line of credit arrangement whereby we may have amounts due from National from time to time. The maximum loan commitment under the line of credit is $2,000,000. At December 31, 2022 and 2021, National did not have an outstanding balance on the line of credit.
The maximum line of credit commitment amount of $2,000,000 is also the amount of a deferred gain that has been outstanding since NHC sold certain assets to National in 1988. The amount of the deferred gain is expected to remain deferred until the management contract with National expires, currently scheduled in January 2028. The deferred gain is included in deferred revenue in the consolidated balance sheets.
Payroll and Related Services
The personnel conducting our business, including our executive management team, are employees of National and may have ownership interests in National only through their participation in the ESOP. National provides payroll services to NHC, provides employee fringe benefits, and maintains certain liability insurance. We pay to National all the costs of personnel employed for our benefit, as well as an administrative fee equal to 1% of payroll costs. The administrative fee paid to National for the years ended December 31, 2022, 2021, and 2020 was $5,074,000, $5,112,000, and $5,026,000, respectively. At December 31, 2022 and 2021, the Company has recorded $74,000 and $2,684,000, respectively, in accounts payable in the consolidated balance sheets as a result of the timing differences between interim payments for payroll and employee benefits services costs.
National’s Ownership of Our Stock
At December 31, 2022, 2021, and 2020, National owns 1,084,763 shares, or approximately 7.1%, 7.0%, and 7.1% of our outstanding common stock, respectively.
Consolidation Considerations
Because of the contractual and management relationships between NHC and National as described in this note above, we have considered whether National should be consolidated by NHC under the guidance provided in ASC Topic 810, Consolidation. We do not consolidate National because (1) NHC does not have any obligation or rights (current or future) to absorb losses or to receive benefits from National. The ESOP participants bear the current and future financial gain or burden of National, (2) National’s equity at risk is sufficient to finance its activities without past or future subordinated support from NHC or other parties, and (3) the equity holders of National (that is collectively the ESOP, its trustees, and the ESOP participants) possess the characteristics of a controlling financial interest, including voting rights that are proportional to their economic interests. Supporting the assertions above is the following: (1) substantive independent trustees are appointed for the benefit of the ESOP participants when decisions must be made that may create the appearance of a conflict of interest between NHC and the ESOP, and (2) National was designed, formed and is operated for the purpose of creating variability and passing that variability along to the ESOP participants—that is, to provide retirement benefits and value to the employees of NHC and NHC’s affiliates. The contractual and management relationships between NHC and National are with the skilled nursing facilities that are substantially less than 50% of the fair value of the total assets of National. NHC does not have a variable interest in National as a whole.
Note 18 – Variable Interest Entity
Accounting guidance requires that a variable interest entity (“VIE”), according to the provisions of ASC Topic 810, Consolidation, must be consolidated by the primary beneficiary. The primary beneficiary is the party that has both the power to direct activities of a VIE that most significantly impact the entity’s economic performance and the obligation to absorb losses of the entity or the right to receive benefits from the entity that could potentially be significant to the VIE. We perform ongoing qualitative analysis to determine if we are the primary beneficiary of a VIE. At December 31, 2022 and 2021, we are the primary beneficiary of one VIE and therefore consolidate that entity.
Springfield, Missouri Lease
In December 2010, we signed an operating agreement to lease Springfield Rehabilitation and Health Care Center, a 120–bed skilled nursing facility located in Springfield, Missouri. The terms of the lease include a ten-year lease and include five additional, five-year lease options as well as a purchase option. The operating lease agreement was established on the same date third party owners purchased the real estate of the 120–bed skilled nursing facility. The third-party owners purchased the real estate for $4,500,000, which is the amount NHC loaned the owners to purchase the facility under the terms of the lease agreement and the mortgage note. The risks and rewards associated with the operations of the facility and any appreciation or deprecation in the value of the real estate of the facility is borne by NHC. A mortgage note receivable from the third-party owners of $11,047,000 at December 31, 2022 and 2021 is eliminated in our consolidated financial statements. Land and buildings and improvements of $11,047,000 at December 31, 2022 and 2021 have been recorded in our consolidated financial statements, as well as the operations of the facility because we are the primary beneficiary in the relationship.
Note 19 – Massachusetts and New Hampshire Skilled Nursing Facilities
On September 1, 2022, we transferred the operations of seven skilled nursing facilities located in Massachusetts and New Hampshire to a third-party operator. NHC leased the real property of these seven facilities from NHI. In conjunction with the transfer of the operations to a third party, we terminated our lease agreement with NHI for the seven skilled nursing facilities and amended our master lease agreement with NHI, see Note 7 – Long-Term Leases.
The seven skilled nursing facilities had net patient revenues of $49,155,000, $67,161,000, and $70,644,000 for the years ended December 31, 2022, 2021, and 2020, respectively. Excluding stimulus funds, the seven skilled nursing facilities had losses before income taxes of $2,478,000, $13,410,000, and $6,569,000 for the years ended December 31, 2022, 2021, and 2020, respectively.
| ITEM 9. |
CHANGES IN AND DISAGREEMENTS WITH ACCOUNTANTS ON ACCOUNTING AND FINANCIAL DISCLOSURE |
None.
| ITEM 9A. |
CONTROLS AND PROCEDURES |
Evaluation of Disclosure Controls and Procedures
Based on their evaluation as of December 31, 2022, the Chief Executive Officer and Principal Accounting Officer of the Company have concluded that the Company’s disclosure controls and procedures (as defined in Rules 13a–15(e) and 15d–15(e) under the Securities Exchange Act of 1934, as amended) were effective to ensure that the information required to be disclosed by us in this Annual Report on Form 10–K was recorded, processed, summarized and reported within the time periods specified in the SEC’s rules and instructions for Form 10–K.
MANAGEMENT’S REPORT ON INTERNAL CONTROL OVER FINANCIAL REPORTING
We are responsible for establishing and maintaining adequate internal control over financial reporting (as defined in Rule 13a–15(f) under the Securities Exchange Act of 1934, as amended). We assessed the effectiveness of our internal control over financial reporting as of December 31, 2022. In making this assessment, our management used the criteria set forth by the Committee of Sponsoring Organizations of the Treadway Commission ("COSO") in Internal Control–Integrated Framework (2013 Framework). We have concluded that, as of December 31, 2022, our internal control over financial reporting is effective based on these criteria. Our independent registered public accounting firm, Ernst & Young, LLP, has issued an attestation report on the effectiveness of the Company’s internal control over financial reporting included herein.
REPORT OF INDEPENDENT REGISTERED PUBLIC ACCOUNTING FIRM
To the Stockholders and Board of Directors of National HealthCare Corporation
Opinion on Internal Control Over Financial Reporting
We have audited National HealthCare Corporation’s internal control over financial reporting as of December 31, 2022, based on criteria established in Internal Control—Integrated Framework issued by the Committee of Sponsoring Organizations of the Treadway Commission (2013 framework) (the COSO criteria). In our opinion, National HealthCare Corporation (the Company) maintained, in all material respects, effective internal control over financial reporting as of December 31, 2022, based on the COSO criteria.
We also have audited, in accordance with the standards of the Public Company Accounting Oversight Board (United States) (PCAOB), the consolidated balance sheets of the Company as of December 31, 2022 and 2021, the related consolidated statements of operations, comprehensive income, equity, and cash flows for each of the three years in the period ended December 31, 2022, and the related notes and financial statement schedule listed in the Index at Item 15(a) and our report dated February 17, 2023 expressed an unqualified opinion thereon.
Basis for Opinion
The Company’s management is responsible for maintaining effective internal control over financial reporting and for its assessment of the effectiveness of internal control over financial reporting included in the accompanying Management’s Report on Internal Control over Financial Reporting. Our responsibility is to express an opinion on the Company’s internal control over financial reporting based on our audit. We are a public accounting firm registered with the PCAOB and are required to be independent with respect to the Company in accordance with the U.S. federal securities laws and the applicable rules and regulations of the Securities and Exchange Commission and the PCAOB.
We conducted our audit in accordance with the standards of the PCAOB. Those standards require that we plan and perform the audit to obtain reasonable assurance about whether effective internal control over financial reporting was maintained in all material respects.
Our audit included obtaining an understanding of internal control over financial reporting, assessing the risk that a material weakness exists, testing and evaluating the design and operating effectiveness of internal control based on the assessed risk, and performing such other procedures as we considered necessary in the circumstances. We believe that our audit provides a reasonable basis for our opinion.
Definition and Limitations of Internal Control Over Financial Reporting
A company’s internal control over financial reporting is a process designed to provide reasonable assurance regarding the reliability of financial reporting and the preparation of financial statements for external purposes in accordance with generally accepted accounting principles. A company’s internal control over financial reporting includes those policies and procedures that (1) pertain to the maintenance of records that, in reasonable detail, accurately and fairly reflect the transactions and dispositions of the assets of the company; (2) provide reasonable assurance that transactions are recorded as necessary to permit preparation of financial statements in accordance with generally accepted accounting principles, and that receipts and expenditures of the company are being made only in accordance with authorizations of management and directors of the company; and (3) provide reasonable assurance regarding prevention or timely detection of unauthorized acquisition, use, or disposition of the company’s assets that could have a material effect on the financial statements.
Because of its inherent limitations, internal control over financial reporting may not prevent or detect misstatements. Also, projections of any evaluation of effectiveness to future periods are subject to the risk that controls may become inadequate because of changes in conditions, or that the degree of compliance with the policies or procedures may deteriorate.
Nashville, Tennessee
February 17, 2023
Changes in Internal Control
There were no changes in our internal control over financial reporting during the quarter ended December 31, 2022 that have materially affected or are reasonably likely to materially affect our internal control over financial reporting.
| ITEM 9B. |
OTHER INFORMATION |
None.
| ITEM 9C. |
DISCLOSURE REGARDING FOREIGN JURISDICTIONS THAT PREVENT INSPECTIONS |
Not Applicable.
PART III
| ITEM 10. |
DIRECTORS, EXECUTIVE OFFICERS AND CORPORATE GOVERNANCE |
The information in our definitive 2023 proxy statement set forth under the captions Directors of the Company and Executive Officers of the Company is hereby incorporated by reference.
| ITEM 11. |
EXECUTIVE COMPENSATION |
The information in our definitive 2023 proxy statement set forth under the caption Compensation Discussion & Analysis is hereby incorporated by reference.
| ITEM 12. |
SECURITY OWNERSHIP OF CERTAIN BENEFICIAL OWNERS AND MANAGEMENT AND RELATED STOCKHOLDER MATTERS |
This information is incorporated by reference from our definitive 2023 proxy statement.
| ITEM 13. |
CERTAIN RELATIONSHIPS AND RELATED TRANSACTIONS AND DIRECTOR INDEPENDENCE |
The information in our definitive 2023 proxy statement set forth under the caption Certain Relationships and Related Transactions is hereby incorporated by reference.
| ITEM 14. |
PRINCIPAL ACCOUNTING FEES AND SERVICES |
The information in our definitive 2023 proxy statement set forth under the caption Report of the Audit Committee is hereby incorporated by reference (which will be filed within 120 days of the end of the fiscal year to which this report relates).
PART IV
| ITEM 15. |
EXHIBITS AND FINANCIAL STATEMENT SCHEDULE |
The following documents are filed as a part of this report:
| (a) |
(1) |
Financial Statements: |
The following financial statements are included in Item 8 of this Annual Report on Form 10-K and are filed as part of this report:
Report of Independent Registered Public Accounting Firm (PCAOB ID:42)
Consolidated Statements of Operations – Years ended December 31, 2022, 2021, and 2020
Consolidated Statements of Comprehensive Income – Years ended December 31, 2022, 2021, and 2020
Consolidated Balance Sheets – At December 31, 2022 and 2021
Consolidated Statements of Cash Flows – Years ended December 31, 2022, 2021, and 2020
Consolidated Statements of Equity – Years ended December 31, 2022, 2021, and 2020
Notes to Consolidated Financial Statements
| |
(2) |
Financial Statement Schedule: |
NATIONAL HEALTHCARE CORPORATION
SCHEDULE II – VALUATION AND QUALIFYING ACCOUNTS
FOR THE YEARS ENDED DECEMBER 31, 2022, 2021, AND 2020
(in thousands)
| Column A | | Column B | | | Column C | | | Column D | | | Column E | |
| | | | | | | Additions | | | | | | | | | |
| Description | | Balance– Beginning of Period | | | Charged to Costs and Expenses | | | Charged to other Accounts | | | Deductions | | | Balance– End of Period | |
| For the year ended December 31, 2020 | | | | | | | | | | | | | | | | | | | | |
| Accrued risk reserves | | $ | 96,011 | | | $ | 86,918 | | | $ | − | | | $ | 83,392 | | | $ | 99,537 | |
| | | | | | | | | | | | | | | | | | | | | |
| For the year ended December 31, 2021 | | | | | | | | | | | | | | | | | | | | |
| Accrued risk reserves | | $ | 99,537 | | | $ | 82,219 | | | $ | − | | | $ | 83,708 | | | $ | 98,048 | |
| | | | | | | | | | | | | | | | | | | | | |
| For the year ended December 31, 2022 | | | | | | | | | | | | | | | | | | | | |
| Accrued risk reserves | | $ | 98,048 | | | $ | 81,743 | | | $ | − | | | $ | 77,322 | | | $ | 102,469 | |
All other financial statement schedules are not required under the related instructions or are inapplicable and therefore have been omitted.
(3) Exhibits:
| EXHIBIT INDEX |
| |
|
|
|
|
| Exhibit No. |
|
Description |
|
Page No. or Location |
| |
|
|
|
|
| 3.1 |
|
Certificate of Incorporation of National HealthCare Corporation |
|
Incorporated by reference to Exhibit 3.1 to the Registrant’s registration statement on Form S–4 (File No. 333–37185) dated October 3, 1997) |
| |
|
|
|
|
| 3.2 |
|
Certificate of Amendment to the Certificate of Incorporation of National HealthCare Corporation |
|
Incorporated by reference to Exhibit 3.5 attached to Form 10-Q filed on August 3, 2017 |
| |
|
|
|
|
| 3.3 |
|
Certificate of Designations of Series A Convertible Preferred Stock of National HealthCare Corporation |
|
Incorporated by reference to Exhibit 2.1 to the current report on Form 8–K filed on December 20, 2006 |
| |
|
|
|
|
| 3.4 |
|
Certificate of Designation Series B Junior Participating Preferred Stock |
|
Incorporated by reference to Exhibit 3.1 to the Registrant’s registration statement on Form 8–A, dated August 3, 2007 |
| |
|
|
|
|
| 3.5 |
|
Restated Bylaws as amended February 14, 2013 |
|
Incorporated by reference to Exhibit 3.5 to the quarterly report on Form 10–Q filed on May 8, 2013. |
| |
|
|
|
|
| 4.1 |
|
Form of Common Stock |
|
Incorporated by reference to Exhibit 4.1 attached to Form 10-Q filed on August 3, 2017 |
| |
|
|
|
|
| 4.2 |
|
Description of each class of securities registered under Section 12 of the Exchange Act |
|
Incorporated by reference to Exhibit 4.2 attached to Form 10-K filed on February 21, 2020 |
| |
|
|
|
|
| 10.1 |
|
Master Agreement of Lease dated as of October 17, 1991 by and among National Health Investors, Inc. and National HealthCorp, L.P. |
|
Incorporated by reference to Exhibit 10.1 to the Registrant's registration statement on Form S–4 filed October 3, 1997 |
| |
|
|
|
|
| 10.2 |
|
Form of Service Agreement by and between National Health Corporation and National HealthCare Corporation |
|
Incorporated by reference to Exhibit 10.5.1 to the Registrant's registration statement on Form S–4 filed October 3, 1997 |
| |
|
|
|
|
| 10.3 |
|
Amendment No. 1 to Master Agreement to Lease between National Health Investors, Inc. and National HealthCorp L.P. |
|
Incorporated by reference to Exhibit 10.19 from 2005 Form 10–K filed March 16, 2006 |
| |
|
|
|
|
| 10.4 |
|
Amendment No. 2 to Master Agreement to Lease between National Health Investors, Inc. and National HealthCare L.P. |
|
Incorporated by reference to Exhibit 10.20 from 2005 Form 10–K filed March 16, 2006 |
| |
|
|
|
|
| 10.5 |
|
Amendment No. 3 to Master Agreement to Lease between National Health Investors, Inc. and National HealthCare L.P. |
|
Incorporated by reference to Exhibit 10.21 from 2005 Form 10–K filed March 16, 2006 |
| |
|
|
|
|
| 10.6 |
|
Amendment No. 4 to Master Agreement to Lease between National Health Investors, Inc. and National HealthCare L.P. |
|
Incorporated by reference to Exhibit 10.22 from 2005 Form 10–K filed March 16, 2006 |
| |
|
|
|
|
| 10.7 |
|
Amendment No. 5 to Master Agreement to Lease between National Health Investors, Inc. and National HealthCare Corporation |
|
Incorporated by reference to Exhibit 10.23 from 2005 Form 10–K filed March 16, 2006 |
| |
|
|
|
|
| *10.8 |
|
National HealthCare Corporation's 2010 Omnibus Equity Incentive Plan |
|
Incorporated by reference to Exhibit A to 2010 Proxy Statement filed April 1, 2010. |
| |
|
|
|
|
| *10.9 |
|
First Amendment dated February 14, 2011 to the National HealthCare Corporation 2010 Omnibus Equity Incentive Plan |
|
Incorporated by reference to Exhibit 10.16 from 2015 Form 10-K filed February 19, 2016. |
| *10.10 |
|
Amendment dated March 10, 2015 to National HealthCare Corporation's 2010 Omnibus Equity Incentive Plan |
|
Incorporated by reference to Appendix A to 2015 Proxy Statement filed April 1, 2015. |
| |
|
|
|
|
| *10.11 |
|
2017 NHC Executive Officer Performance Based Compensation Plan |
|
Incorporated by reference to Appendix B to 2017 Proxy Statement filed April 4, 2017. |
| |
|
|
|
|
| * 10.12 |
|
National HealthCare Corporation’s 2020 Omnibus Equity Incentive Plan |
|
Incorporated by reference to Appendix A to 2020 Proxy Statement filed April 6, 2020 |
| |
|
|
|
|
| 10.13 |
|
Amendment to Purchase and Sale Agreement with Modifications to Master Agreement to Lease between National Health Investors, Inc. and National HealthCare Corporation |
|
Incorporated by reference to Exhibit 10.1 of National HealthCare Corporation's Form 10–Q filed on November 5, 2013 |
| |
|
|
|
|
| 10.14 |
|
Agreement to Lease between NHI–REIT of Northeast, LLC, Landlord and NHC/OP, L.P. and National HealthCare Corporation, Co–Tenants |
|
Incorporated by reference to Exhibit 10.4 of National HealthCare Corporation's Form 10–Q filed on November 5, 2013 |
| |
|
|
|
|
| 10.15 |
|
Amended and Restated Amendment No. 6 to Master Agreement to Lease between National Health Investors, Inc. and National HealthCare Corporation |
|
Incorporated by reference to Exhibit 10.2 of National HealthCare Corporation's Form 10–Q filed on November 5, 2013 |
| |
|
|
|
|
| 10.16 |
|
Amendment No. 7 to Master Agreement to Lease between National Health Investors, Inc. and National HealthCare Corporation |
|
Incorporated by reference to Exhibit 10.3 of National HealthCare Corporation's Form 10–Q filed on November 5, 2013 |
| |
|
|
|
|
| 10.17 |
|
Contribution Agreement dated December 29, 2011 between National HealthCare Corporation and Caris HealthCare, L.P. pursuant to which NHC acquired a 7.5% interest in Caris from McRae in exchange for $7,500,000 |
|
Incorporated by reference to Exhibit 10.26 to National HealthCare Corporation's annual report on Form 10–K filed on February 21, 2014 |
| |
|
|
|
|
| 10.18 |
|
Assignment of membership interest in Solaris Hospice, LLC dated December 29, 2011 and effective on January 1, 2012, whereby NHC assigned its membership interest to Caris in exchange for an additional 2.7% limited partnership interest in Caris. |
|
Incorporated by reference to Exhibit 10.27 to National HealthCare Corporation's annual report on Form 10–K filed on February 21, 2014 |
| |
|
|
|
|
| 10.19 |
|
Purchase and Sale Agreement and Extension of Master Lease dated December 26, 2012 between National Health Investors, Inc. and National HealthCare Corporation |
|
Incorporated by reference to Exhibit 10.29 to National HealthCare Corporation's annual report on Form 10–K filed on February 21, 2014 |
| |
|
|
|
|
| 10.20 |
|
Amendment No. 8 to Master Agreement to Lease between National Health Investors, Inc. and National HealthCare Corporation |
|
Incorporated by reference to Exhibit 10.20 to National HealthCare Corporations annual report on Form 10-K Filed on February 19, 2021 |
| |
|
|
|
|
| 10.21 |
|
Purchase and Sale Agreement dated June 11, 2021 between NHC/OP, L.P., a wholly owned subsidiary of NHC, and Norman C. McRae and McRae Investment Company, LLC |
|
Incorporated by reference to Exhibit 10.21 to National HealthCare Corporation annual report on Form 10-K Filed on February 18, 2022 |
| |
|
|
|
|
| 10.22 |
|
Amendment No. 9 to Master Agreement to Lease between National Health Investors, Inc. and National HealthCare Corporation |
|
Incorporated by reference to Exhibit 10.1 of National HealthCare Corporation's Form 10-Q filed on November 3, 2022 |
| |
|
|
|
|
| 10.23 |
|
Amendment No. 10 to Master Agreement to Lease between National Health Investors, Inc. and National HealthCare Corporation |
|
Incorporated by reference to Exhibit 10.2 of National HealthCare Corporation's Form 10-Q filed on November 3, 2022 |
| |
|
|
|
|
| 14 |
|
Code of Ethics of National HealthCare Corporation |
|
Available at NHC’s website www.nhccare.com or in print upon request to: National HealthCare Corp. Attn: Investor Relations P. O. Box 1398 Murfreesboro, TN 37133–1398 Telephone (615) 890–2020 |
| |
|
|
|
|
| 21 |
|
Subsidiaries of Registrant |
|
Filed Herewith |
| |
|
|
|
|
| 23 |
|
Consent of Independent Registered Public Accounting Firm – Ernst & Young LLP |
|
Filed Herewith |
| *Indicates management contract or compensatory plan or arrangement. |
SIGNATURES
Pursuant to the requirements of Section 13 or 15(d) of the Securities Exchange Act of 1934, the Registrant has duly caused this report to be signed on its behalf by the undersigned, thereunto duly authorized.
| |
NATIONAL HEALTHCARE CORPORATION |
| |
|
| Date: February 17, 2023 |
BY: /s/ Stephen F. Flatt |
| |
Stephen F. Flatt |
| |
Chief Executive Officer and Director |
Pursuant to the requirements of the Securities Exchange Act of 1934, this Report has been signed below by the following persons on behalf of the registrant and in the capacities and on the dates indicated.
| Date: February 17, 2023 |
/s/ Stephen F. Flatt |
| |
Stephen F. Flatt |
| |
Chief Executive Officer and Director |
| |
(Principal Executive Officer) |
| |
|
| Date: February 17, 2023 |
/s/ Brian F. Kidd |
| |
Brian F. Kidd |
| |
Senior Vice President and Controller |
| |
(Principal Financial Officer) |
| |
(Principal Accounting Officer) |
| |
|
| Date: February 17, 2023 |
/s/ Robert G. Adams |
| |
Robert G. Adams |
| |
Chairman of the Board |
| |
|
| Date: February 17, 2023 |
/s/ J. Paul Abernathy |
| |
J. Paul Abernathy |
| |
Director |
| |
|
| Date: February 17, 2023 |
/s/ W. Andrew Adams |
| |
W. Andrew Adams |
| |
Director |
| |
|
| Date: February 17, 2023 |
/s/ Ernest G. Burgess |
| |
Ernest G. Burgess |
| |
Director |
| |
| Date: February 17, 2023 |
/s/ Emil E. Hassan |
| |
Emil E. Hassan |
| |
Director |
| |
|
| Date: February 17, 2023 |
/s/ Sandra Y. Trail |
| |
Sandra Y. Trail |
| |
Director |
| |
|
| Date: February 17, 2023 |
Richard F. LaRoche, Jr. |
| |
Director |